Miscarriage
Why Too Many Sperms Spoil the Egg
Unusually high sperm numbers overwhelm the egg and disrupt fertilization.
Posted August 11, 2017 Reviewed by Ekua Hagan
Well-documented reports spanning 25 years have yielded mounting evidence that sperm counts are tumbling in industrialized countries. (See my April 20, 2017 post Going, Going, Gone? Human Sperm Counts Are Plunging.)
A fall of over 50 percent in counts over a 40-year period has at last triggered active media interest, provoking dire warnings of looming human extinction. Although many see this as good news for the planet, it is unlikely to happen fast enough. Moreover, this story has a rarely mentioned flip-side: Little-discussed findings indicate that too many sperms can also harm fertility.
Fertilization by more than one sperm
It is widely known that fertilization of a mammal egg by more than one sperm (polyspermy) has catastrophic effects. When sex cells (eggs and sperms) are produced, the usual number of chromosomes is halved. Human body cells typically have 46 chromosomes (diploid number), but a sex cell contains only 23 (haploid number).
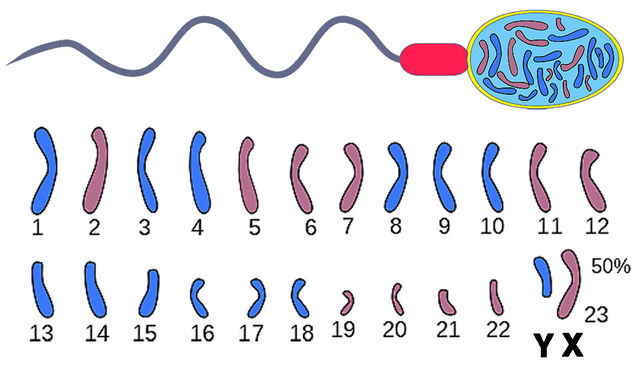
A sex cell contains only a single sex chromosome, X in an egg and X or Y in a sperm. Fusion of a sperm with an egg at fertilization restores the normal chromosome number, and approximately equal numbers of female (XX) and male (XY) offspring are produced.
If two sperms fertilize an egg, things go wildly wrong, yielding a triploid offspring with 69 chromosomes with an extra set in addition to the normal maternal/paternal pair.
An egg fertilized by three sperms receives two extra chromosome sets, resulting in a quadruploid individual with 92 chromosomes. Extra chromosome sets directly harm sex determination. A triploid individual, for instance, has an abnormal combination of sex chromosomes (XXX, XXY or XYY).
It might be thought that all animals possess effective mechanisms to prevent fertilization of an egg by more than one sperm. However, in at least some fish and bird species several sperms actually fertilize the egg. Only afterward do special mechanisms make sure that just one set of male chromosomes contributes to the offspring.
So why is single-sperm fertilization of the egg the rule for mammals? A connection has been suggested with the tiny size of the mammal egg, which is extremely small because it contains no yolk.
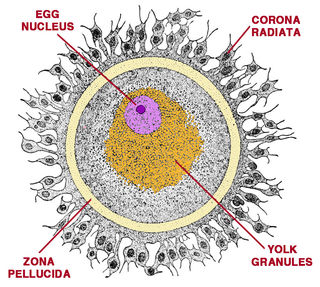
Whatever the reason, once the egg has been fertilized, two surrounding layers—the clear outer zona pellucida and the underlying egg membrane—usually prevent additional sperms from entering.
Too many sperms linked to miscarriage
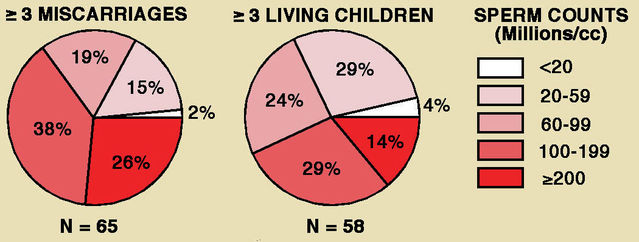
John MacLeod and Ruth Gold provided an early indication of a downside to high sperm counts in a 1957 paper. They compared semen quality between men whose wives experienced repeated miscarriage and men who had fathered at least three normal living children without intervening failed pregnancies.
Surprisingly, semen quality was higher in the miscarriage group. Men in that group had significantly higher sperm concentrations (averaging over 100 million/ml) and more motile sperms (averaging over 60 percent). Almost twice as many (26 percent versus 14 percent) had sperm concentrations exceeding 200 million/ml.
MacLeod and Gold also noted that almost a third of men who produced four or more living children without failed pregnancies had only moderate sperm concentrations (20-59 million/ml).
Much later, in 1975, Naghma-E-Rehan and colleagues published an analysis of semen samples collected before vasectomy from 1,300 men who had fathered at least two children. Sperm concentrations ranged widely, from 1.5 to 375 million/ml, averaging 65 million/ml.
Fifteen men (just over 1 percent) had extraordinarily high values. In this extreme condition, known as polyzoospermy in medical circles, sperm concentrations surpass 250 million/ml and total sperm count exceed 800 million. The spouses of six of these men (40 percent) had experienced at least one miscarriage, compared with an overall rate of 7 percent.
For wives of 25 men who had sperm counts below 10 million/ml, but had fathered two or more children, the rate was only 4 percent.
Several studies of fetal material from miscarriages have shown that major chromosomal abnormalities are often present.
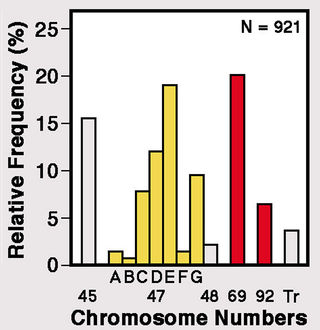
In 1975, Joëlle Boué and colleagues published a landmark study of 1,500 cases. By analyzing relative frequencies of the different types of chromosome anomaly, they estimated that some kind of aberration occurs in half of all conceptions.
Among those aberrations, about 20 percent had 69 chromosomes (triploidy), which could arise from two sperms fertilizing an egg, while another 6 percent had 92 chromosomes (quadruploidy), potentially indicating three fertilizing sperms.
Fetuses with additional chromosome sets
Fertilization of an egg by two sperms results in the presence of a triploid chromosome set, including three sex chromosomes. This condition can, however, arise in two other ways.
First — because of a developmental error — a sperm may occasionally have two chromosome sets instead of the usual one. Such a sperm fertilizing an egg by would yield a triploid condition. Second, an abnormal egg with two chromosome sets might be fertilized by a normal sperm.
Several medical studies have yielded direct evidence of double fertilization of human eggs, generally with fatal consequences. Almost all conceptions with triploidy are eliminated in the womb, and the few that make it to birth survive for just a few hours.
A 1977 report from Nora Blackwell and colleagues described an infant with multiple severe abnormalities that died soon after birth. It was found to have 69 chromosomes, including three sex chromosomes (XXY). Features of certain chromosomes that could only have come from the father convincingly indicated that two sperms had fertilized the egg.
Soon afterward, Patricia Jacobs and colleagues followed this single case report with an overview of the origins of human triploids. Their groundbreaking 1978 paper surveyed all miscarriages over two years in a Hawaiian maternity hospital. For 21 out of 26 miscarried fetuses with triploidy, they were able to identify the source of the additional chromosomes. An additional chromosome set came from the father in 17 cases and from the mother in 3, with one case left unresolved. Further calculations indicated that two-thirds of the triploids resulted from fertilization by two sperms, a quarter from fertilization by a single sperm with a double set of chromosomes and only 1 in 10 from a normal sperm penetrating an egg possessing two sets of chromosomes. Jacobs and colleagues noted that triploidy is relatively common in humans, estimating that it affects 1 percent to 3 percent of all detectable conceptions.
Benefiting from more advanced techniques, in 2000 Qinghua Shi and René Martin reported findings for aberrant chromosome numbers in over 200,000 sperms from 10 healthy Chinese men compared with a similar sample from 10 healthy Canadians. The mean frequency of diploid sperms containing 46 chromosomes was notably low, less than 0.4 percent. Despite marked differences between donors in the occurrence of diploid sperms, there was no overall distinction between Chinese and Canadian men.
Also in 2000, Michael Zaragoza and colleagues reported on a study of parental origin of chromosomes in 91 miscarriages with triploidy. They confirmed that most cases were attributable to fertilization of the egg by two sperms.
Implications of polyspermy
There is, then, clear evidence that men can produce too many sperms, not just too few. But discussions of sperm numbers in humans and other mammals generally focus exclusively on the need for large numbers, with no reference to the risk of excessive sperm concentrations that can threaten fetal development. For this reason, current one-sided notions of “sperm competition” will need careful re-examination.
As sperm expert Michael Bedford noted in a perceptive 2008 paper, “...one should be wary of the concept that there is a ‘race’ to reach unfertilized eggs as a function of the sperm’s velocity, and of media images showing many sperm supposedly competing for an unfertilized egg."
References
Bedford, J.M. (2008) Puzzles of mammalian fertilization — and beyond. International Journal of Developmental Biology 52:415-426.
Blackwell, N.J., Keeling, J.W. & Lindenbaum, R.H. (1977) Dispermic origin of a 69, XXY triploid. Human Genetics 32:121-124.
Boué, J., Boué, A. & Lazar, P. (1975) Retrospective and prospective epidemiological studies of 1500 karyotyped spontaneous human abortions. Teratology 12:11-26.
Gardner, A.J. & Evans, J.P. (2006) Mammalian membrane block to polyspermy: new insights into how mammalian eggs prevent fertilisation by multiple sperm. Reproduction, Fertility & Development 18:53-61.
Hunter, R.H.F. (1996) Ovarian control of very low sperm/egg ratios at the commencement of mammalian fertilization to avoid polyspermy. Molecular Reproduction and Development 44:417-422.
MacLeod, J. & Gold, R.Z. (1957) The male factor in fertility and infertility. IX. Semen quality in relation to accidents of pregnancy. Fertility & Sterility 8:36-49.
Naghma-E-Rehan, Sobrero, A.J. & Fertig, J.W. (1975) The semen of fertile man: statistical analysis of 1300 men. Fertility & Sterility 26:492-502.
Shi, Q. & Martin, R.H. (2000) Spontaneous frequencies of aneuploid and diploid sperm in 10 normal Chinese men: assessed by multicolor fluorescence in situ hybridization. Cytogenetics & Cell Genetics 90:79-83.
Snook, R.R., Hosken, D.J. & Karr, T.L. (2011) The biology and evolution of polyspermy: Insights from cellular and functional studies of sperm centrosome; behaviour in the fertilised egg. Reproduction 142:779-792.
Zaragoza, M.V., Surti, U., Redline, R.W., Millie, E., Chakravarti, A. & Hassold, T.J. (2000) Parental origin and phenotype of triploidy in spontaneous abortions: Predominance of diandry and association with the partial hydatidiform mole. American Journal of Human Genetics 66:1807-1820.




