Health
Going, Going, Gone? Human Sperm Counts Are Plunging
Recent findings confirm declining sperm counts linked to male health problems.
Posted April 20, 2017
Are human sperm counts crashing? Despite numerous careful analyses indicating falling numbers, opposing reports still appear occasionally and doubts persist. Accumulated evidence has revealed that the apparent conflict between reports may in part be due to different onset times in different places. And mounting medical evidence also shows that men’s reproductive health problems—ranging from failed testis descent to cancers—are increasing in tandem.
Initial reports of falling sperm counts
Kinloch Nelson and Raymond Bunge first reported a marked decrease in human sperm counts in 1974. Ejaculates from almost 400 American men opting for vasectomy over the period 1968-1972 revealed average total sperm counts below 140 million. This was far below the average of over 300 million that earlier investigators reported. Nelson and Bunge checked semen assessments for 400 men who underwent infertility evaluation in their own clinic in 1956-1958 and found comparably high counts.
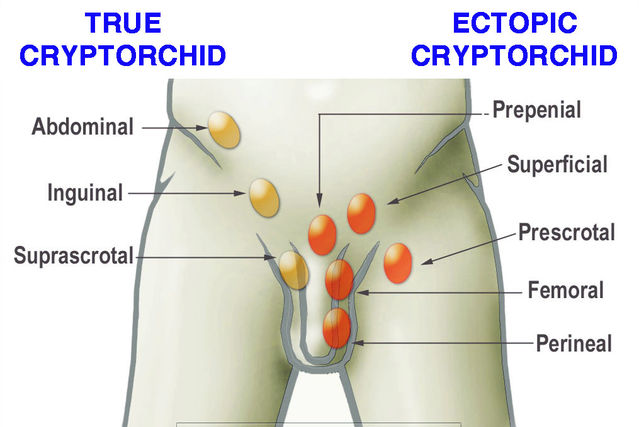
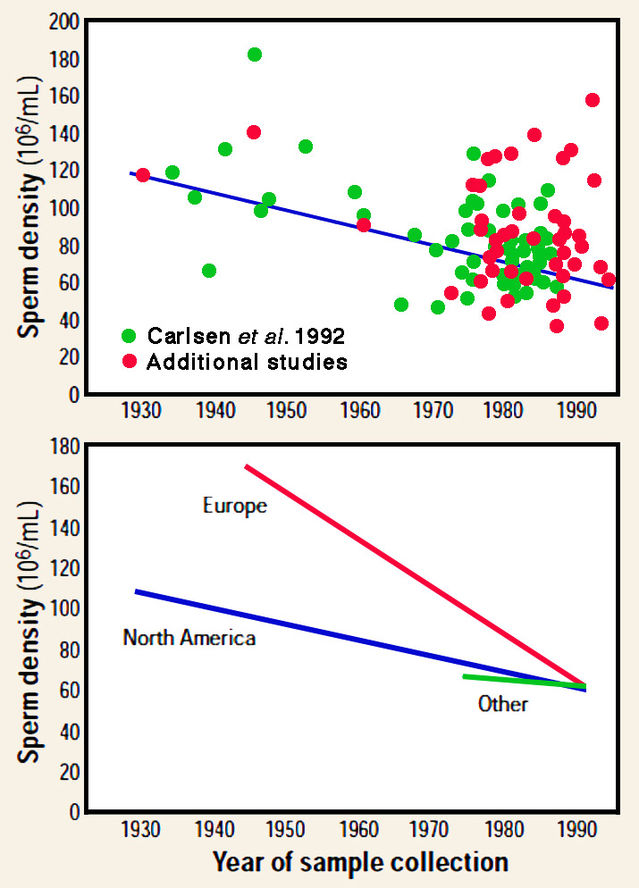
In 1992 an overarching analysis of accumulated data by Elisabeth Carlsen and colleagues dramatically expanded that original finding. Carefully selecting reports on men with no history of infertility, they reviewed results from 61 papers published between 1938 and 1991 for an overall total of 15,000 men. The outcome, after excluding various possible sources of bias, was that average sperm counts had been approximately halved over the 50-year period 1940-1990. Carlsen and colleagues also noted the alarming fact that an increase in medical issues concerning the male reproductive system was occurring in tandem with declining sperm counts: failed descent of testes (cryptorchidism), penis malformation with the urethra opening on the underside before the tip (hypospadias) and cancers of testes and prostate gland.
Findings questioned
Carlsen and colleagues’ conclusion that human sperm counts had fallen drastically since the 1950s triggered an animated controversy. Opening the debate soon afterwards, Ian Tummon and David Mortimer challenged the validity of the results. In particular, they noted likely changes in methods and quality control over time and claimed that the apparent downward trend could be due to a shift to generally lower sperm counts after 1961. Although this challenge is, at first sight, unsettling, a 1997 paper veterinarian Brian Setchell neatly demolished it. Over the same period, directly comparable methods have been routinely used to evaluate semen in farm animals, so their sperm counts should show a similar decline in response to any change in procedures. When Setchell reviewed sperm counts over a 60-year period starting in the early 1930s, he found no change for either cattle or pigs and a slight, but significant, increase in sheep. Crucially, Setchell noted that any decline in human sperm counts must be due to factors that do not affect these farm animals.
More recent studies
A larger-scale overview published in 2000 by Shanna Swan and colleagues confirmed and reinforced the 1992 findings reported by Carlsen and colleagues. The original dataset was expanded to a total of 101 sources published between 1934 and 1996. After controlling for possible confounding factors, the overall decline in sperm count over that 62-year interval was virtually identical to that reported by Carlsen and colleagues. However, data analysed in that previous study came predominantly from Europe and North America, whereas Swan and her team were able to include more information from non-Western countries. Separate analyses confirmed that marked declines had occurred in both the USA and Europe, whereas studies from other countries showed no downward trend. It therefore seemed that the decline was linked to industrialization.
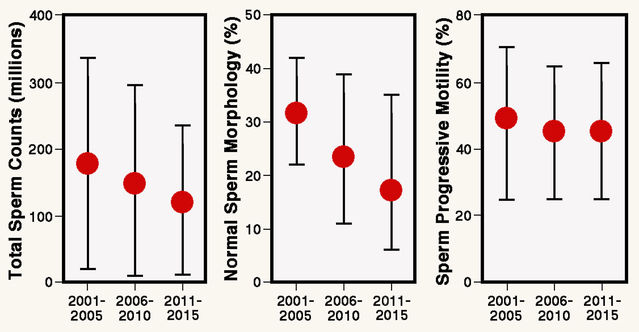
Most recently, in a 2017 paper, Chuan Huang and colleagues reported results of semen analysis for 30,636 young sperm donors in Hunan Province, China for 2001-2015. Median values for total sperm counts showed a highly significant decline over that 15-year period from 182 to 119 million per ejaculate. Alarmingly, the proportion of qualified donors fell by two thirds from 56% in 2001 to 18% in 2015. This study is important because it clearly shows that declining sperm counts are also occurring in Asia.
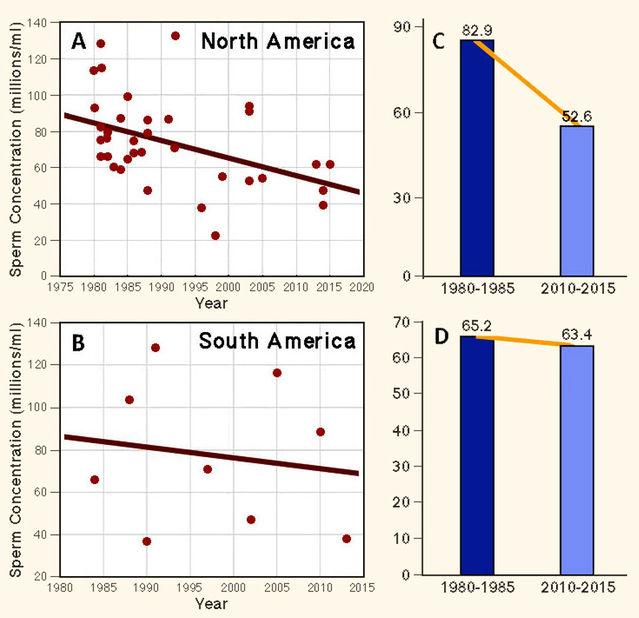
Last but not least, in 2016 Pallav Sengupta and colleagues published a welcome overview of 138 reports dating between 1980 and 2015, emphasizing potential geographical differences. Analysis revealed a highly significant overall 57% decrease in average sperm concentration over that 35-year period. Separate consideration of individual geographical regions identified significant declines in North America, Europe, Asia and Africa, contrasting with a significant upward trend in sperm counts that emerged for Australia.
Sperm counts and fertility
It is reasonable to conclude that human sperm counts are definitely decreasing in many parts of the world. The next logical question is whether lower sperm counts have already diminished male fertility.
It has been known since the 1950s that men are often infertile if total sperm counts per ejaculate remain persistently below 70 million. In 1953, Edward Tyler reported that conception rates progressively improved as total sperm counts increased from 70 million to 200 million per ejaculate, whereas no further improvement occurred above that level. A 2002 paper by Rémy Slama and colleagues confirmed this finding. They examined the relationship between sperm counts and time to pregnancy in almost 1,000 couples in four European cities. Pregnancy was achieved increasingly rapidly up to a total sperm count of about 200 million, but not beyond that level. Vast numbers of sperms are evidently needed for normal male fertility, and as sperm counts decline men are increasingly drifting below the threshold of 60 million sperms, into a range where fertility is surely affected.
Hormone mimics
Environmental factors are undoubtedly responsible for markedly declining sperm counts accompanied by increasing abnormalities of the male sex organs and cancers over the last 80 years. Prime suspects are organic compounds with hormone-like activity (endocrine disruptors), graphically described as “imposters” by Theo Colborn, Dianne Dumanoski and John Peterson Myers in their superb 1997 book Our Stolen Future. Results from experimental studies of laboratory mammals combined with epidemiological evidence from human subjects agree in making that link. Although some well-known endocrine disruptors, notably DDT and DES, have been officially recognized and controlled, many others, such as Bisphenol A (BPA) have appeared on the scene. (See my blog post "Spectators on Steroids".) In a comprehensive review paper published in 2016, Nils Skakkebæk and colleagues reviewed the evidence implicating endocrine disruptors in declining sperm counts and increasing male reproductive problems. In fact, in 2001 the Skakkebæk team—one of the first to raise the alarm about falling sperm counts—coined the term testicular dysgenesis syndrome to include low semen quality, high and possibly increasing frequencies of cryptorchidism and hypospadias, and a rising incidence of testicular cancer.
A fundamental point is that endocrine disruptors have two distinct modes of action. The most obvious is their direct impact on males after puberty. Epidemiological studies have, for instance, identified an association between semen quality in men and environmental exposure to BPA in the workplace. But a less obvious—and more insidious—mode of action is in the womb, where endocrine disruptors in the mother’s bloodstream can disrupt embryonic and fetal development, notably during formation of the sex organs. This double-barrelled effect may explain some of the differences seen between studies conducted in different contexts.
References
Readers are encouraged to visit the website of The Endocrine Disruption Exchange (TEDX: http://www.endocrinedisruption.com/home.php) and to watch an excellent video by its late Founder, Dr. Theo Colborn, discussing the general problem of endocrine disruptors in the environment.
Carlsen, E., Giwercman, A., Keiding, N. & Shakkebaek, N.E. (1992) Evidence for decreasing quality of semen during past 50 years. British Medical Journal 305:609-613.
Colborn, T., Dumanoski, D. & Myers, J. P. (1997) Our Stolen Future: Are We Threatening our Fertility, Intelligence and Survival? (Paperback Version with Epilogue). New York: Dutton.
Huang, C., Li, B., Xu, K., Liu, D.., Hu, J., Yang, Y., Nie, H.-C., Fan, L. & Zhu, W. (2017) Decline in semen quality among 30,636 young Chinese men from 2001 to 2015. Fertility & Sterility 107:83-88.
Mendiola, J., Jørgensen, N., Mínguez-Alarcón, L., Sarabia-Cos, L., López-Espín, J.J., Vivero-Salmerón, G., Ruiz-Ruiz, K.J., Fernández, M.F., Olea, N., Swan, S.H. & Torres-Cantero, A.M. (2013) Sperm counts may have declined in young university students in Southern Spain. Andrology 1:408-413.
Nelson, C.M.K. & Bunge, R.G. (1974) Semen analysis: evidence for changing parameters of male fertility potential. Fertility & Sterility 25:503-507.
Sengupta, P., Dutta, S. & Krajewska-Kulak, E. (2016) The disappearing sperms: Analysis of reports published between 1980 and 2015. American Journal of Men's Health 1-27. DOI: 10.1177/1557988316643383
Setchell, B.P. (1997) Sperm counts in semen of farm animals 1932-1995. International Journal of Andrology 20:209-214.
Skakkebaek, N.E., Rajpert-De Meyts, E., Buck Louis, G.M., Toppari, J., Andersson, A.-M., Eisenberg, M.L., Jensen, T.K., Jørgensen, N., Swan, S.H., Sapra, K.J., Ziebe, S., Priskorn, L. & Juul, A. (2016) Male reproductive disorders and fertility trends: Influences of environment and genetic susceptibility. Physiological Reviews 96:55-97.
Skakkebæk, N.E., Rajpert-De Meyts, E. & Main, K.M. (2001) Testicular dysgenesis syndrome: an increasingly common developmental disorder with environmental aspects. Human Reproduction 16:972-978.
Slama, R., Eustache, F., Ducot, B., Jensen, T.K., Jørgensen, N., Horte, A., Irvine, S., Suominen, J., Andersen, A.G., Auger, J., Vierula, M., Toppari, J., Andersen, J.N., Keiding, N., Skakkebæk, N.E., Spira, A. & Jouannet, P. (2002) Time to pregnancy and semen parameters: a cross-sectional study among fertile couples from four European cities. Human Reproduction 17:503-515.
Swan, S.H., Elkin, E.P. & Fenster, L. (2000) The question of declining sperm density revisited: An analysis of 101 studies published 1934-1996. Environmental Health Perspectives 108:961-966.
Tummon, I.S. & Mortimer, D. (1992) Decreasing quality of semen. British Medical Journal 305:1228-1229.
Tyler, E.T. (1953) Physiological and clinical aspects of conception. Journal of the American Medical Association 153:1351-1356.




