Health
3 Brain-Protective Lifestyle Hacks
How to take advantage of the link between Alzheimer’s disease and the gut.
Posted August 4, 2022 Reviewed by Hara Estroff Marano
Key points
- Alzheimer's disease fatalities have increased 150% since 2000.
- Neuroinflammation, beta amyloid plaque accumulation, and tau protein tangles are considered causative.
- Gut dysbiosis has been associated with the development of neurodegenerative disorders including Alzheimer's.
- Simple lifestyle shifts can help prevent development of Alzheimer's disease.
By Nicole Cain, ND, MA

Alzhiemer’s disease (AD), a neurodegenerative condition characterized by cognitive and behavioral impairment, is estimated to be at the foundation of as many as 80% of dementia cases.1 Projections indicate that more than 140 million individuals across the globe will be suffering from the condition by 2050.2 In the United States alone, reported deaths from Alzheimer’s disease increased nearly 150% between 2000 and 2018, for an annual total of more than 120,000.3
Although research is ongoing, the cause of and contributing factors to AD development and progression are still unclear. One of the most common hypotheses cites excessive buildup of beta amyloid (Aβ) plaques in the brain.4 The plaques cause damage to brain cells (neuron) and, ultimately, death. Current thinking focuses on inadequate Aβ clearance, rather than overproduction, as a causative factor.5 Additional work indicates that neuronal damage and related cognitive changes may be detected prior to excessive buildup of beta amyloid.6
Another hypothesis posits that the disease is closely related to abnormalities in the structure and function of the brain’s tau protein, a substance that helps to stabilize the internal skeleton of nutrient-delivering microtubules in the nerve cells (neurons) in the brain.7,8,9 When abnormal chemical changes occur, tau proteins detach from the microtubules and cling together forming neurofibrillary tangles.10
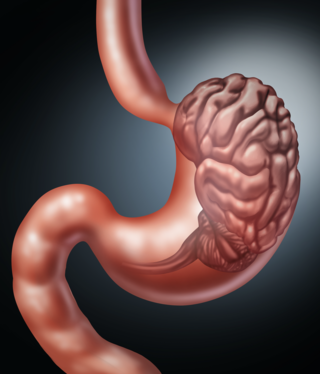
Research also suggests that the gut-brain axis plays a role in the development of neurodegenerative diseases, including Alzheimer’s.
The Gut Microbiome’s Role in AD
Animal and human models have revealed that the gut microbiome plays an essential role in healthy neurological activity. For example, the gut regulates metabolism of short-chain fatty acid (SCFA), brain-derived neurotrophic factor (BDNF), and production of other neuroactive molecules and neurotransmitters.6
Microbes in the gut also influence the brain through neurological, hormonal, metabolic, and immune system interaction. In fact, a 2022 review describes a distinct microbial “signature” that can reliably differentiate high-level Aβ Alzhiemer’s disease patients from normal controls. Preclinical studies have even shown that changes in the microbiome may offer predictive value into disease progression in high-risk AD patients prior to Aβ buildup.6
Often the foundational dysfunction in the gut-brain axis is linked to intestinal permeability, commonly known as “leaky gut.” The condition occurs, in part, as a result of inflammation in the gastrointestinal system related to a dysbiotic gut microbiome. Damage to intestinal cells increases the likelihood that undesirable microbes and toxins (e.g. lipopolysaccharides, or LPS) will escape the intestinal lumen and set off a body-wide inflammatory response.
The systemic inflammation can lead to erosion of the blood brain barrier (BBB) that normally shields the brain from circulating toxins and other undesirable substances—esulting in pathogens and toxins “leaking” into the brain. Further, research reveals that LPS in the brain contributes to the development of plaques, as do amyloids produced by gut bacteria, when the BBB is compromised.6
Fortunately, there are very simple lifestyle interventions that may help prevent the onset and progression of Alzheimer’s and similar diseases.
3 Simple Lifestyle Hacks to Protect the Brain
1. Feed the Good Bugs in the Gut
A gut-friendly diet of whole foods high in fiber has consistently proven to be an effective approach to supporting microbiome balance and brain health; it fosters production of cognition-supporting substances.11 The standard American diet, high in red meat and highly processed foods, is typically bereft of such capabilities. Eating plenty of colorful, plant-based dishes feeds the good bugs of the microbiome and provides needed micronutrients. Including a quality prebiotic for extra microbiome support is a great approach. If dysbiosis is suspected, a regimen of quality nutritional supplements including omega-3 fatty acids, glutathione, zinc, and collagen has been clinically shown to help seal and heal the gut.12
2. Balance the Gut Microbiome Population
Many studies have evaluated the benefits of quality probiotic supplementation to support gut microbiome diversity and the gut-brain axis. A 2019 clinical trial looked at inflammation and cognitive function in two groups of AD patients: The first group received probiotic strains of L. acidophilus, B. bifidum, and B. longum along with selenium over a period of three months, with the placebo group serving as a control. Those taking the probiotics and selenium demonstrated reduced inflammation and increased cognitive function.13 Other recent studies14,15 add evidence that quality probiotic and prebiotic supplementation may offer an effective strategy for supporting the gut-brain axis and preventing the pathological changes associated with neurodegenerative diseases like AD.
“The latest research results…clearly show that oral administration of probiotic bacteria such as bifidobacteria and lactic acid bacteria in AD disease reduces cognitive deficits by reducing inflammation or the amount of Aβ accumulated in the brain structures.” Wiatrek, et al. 2022.
Selection of a reliably effective probiotic formulation however, can be challenging. Multistrain probiotics offer the benefit of inter-strain synergies and additive beneficial effects,16 which may provide more comprehensive support. But not all probiotic strains work well together. The best approach to selecting a brain health-optimized product is to ensure that the final formulation is supported by independent human clinical evidence of efficacy. Probiotic companies with this level of performance evidence make the research readily available for review.17
3. Stay Active
The myriad benefits of regular physical exercise are incontrovertible, including its healthful influence on both the mind and the microbiome. Regular movement and exercise such as running on a treadmill or daily walking can produce positive results for seniors including those suffering from the cognitive symptoms of AD.20,21 Making activity a lifestyle pays off in physical strength, energy, and long-term cognitive clarity.
Final Thoughts
Although many neurodegenerative diseases, including and especially Alzheimer’s disease, is on the increase,3 small shifts toward better gut-microbiome health can play a strong preventative role.
References
Pflanzner T, Kuhlmann CR, Pietrzik CU. Blood-brain-barrier models for the investigation of transporter- and receptor-mediated amyloid-β clearance in Alzheimer's disease. Curr Alzheimer Res. 2010 Nov;7(7):578-90. doi: 10.2174/156720510793499066. PMID: 20704558.
Tiwari S, Atluri V, Kaushik A, Yndart A, Nair M 2019 Alzheimer's disease: pathogenesis, diagnostics, and therapeutics Int J Nanomedicine 14 5541–5554
Alzheimer’ s Association Report, 2020 Alhzheimer’s disease facts and figures, Mar 2020.
Selkoe DJ, Hardy J. The amyloid hypothesis of Alzheimer's disease at 25 years. EMBO Mol Med. 2016 Jun 1;8(6):595-608. doi: 10.15252/emmm.201606210. PMID: 27025652; PMCID: PMC4888851.
Zhang, Yan-Li1,2; Wang, Juan1; Zhang, Zhi-Na3; Su, Qiang1,*; Guo, Jun-Hong1,*. The relationship between amyloid-beta and brain capillary endothelial cells in Alzheimer’s disease. Neural Regeneration Research: November 2022 - Volume 17 - Issue 11 - p 2355-2363 doi: 10.4103/1673-5374.335829
Wiatrak B, Balon K, Jawień P, Bednarz D, Jęśkowiak I, Szeląg A. The Role of the Microbiota-Gut-Brain Axis in the Development of Alzheimer's Disease. Int J Mol Sci. 2022 Apr 27;23(9):4862. doi: 10.3390/ijms23094862. PMID: 35563253; PMCID: PMC9104401.
Kelsey R. Thomas, Katherine J. Bangen, Alexandra J. Weigand, Emily C. Edmonds, Christina G. Wong, Shanna Cooper, LisaDelano-Wood, Mark W. Bondi, for the Alzheimer's Disease Neuroimaging Initiative, Neurology Jan 2020, 94 (4) e397-e406; DOI:10.1212/WNL.0000000000008838
Ismail, R., Parbo, P., Madsen, L.S. et al. The relationships between neuroinflammation, beta-amyloid and tau deposition in Alzheimer’s disease: a longitudinal PET study. J Neuroinflammation 17, 151 (2020). https://doi.org/10.1186/s12974-020-01820-6
Chen, Y., Fang, L., Chen, S., Zhou, H., Fan, Y., Lin, L., et al. (2020). Gut microbiome alterations precede cerebral amyloidosis and microglial pathology in a mouse model of Alzheimer’s Disease. Biomed. Res. Int. 2020:8456596. doi: 10.1155/ 2020/8456596
National Institute of Aging, What Happens to the Brain in Alzheimer’s Disease.
Sandhu, K.V.; Sherwin, E.; Schellekens, H.; Stanton, C.; Dinan, T.G.; Cryan, J.F. Feeding the microbiota-gut-brain axis: Diet,microbiome, and neuropsychiatry. Transl. Res. 2017, 179, 223–244
Camilleri M. Leaky gut: mechanisms, measurement and clinical implications in humans. Gut. 2019 Aug;68(8):1516-1526. doi: 10.1136/gutjnl-2019-318427. Epub 2019 May 10. PMID: 31076401; PMCID: PMC6790068
Tamtaji, O.R.; Heidari-soureshjani, R.; Mirhosseini, N.; Kouchaki, E.; Bahmani, F.; Aghadavod, E.; Tajabadi-Ebrahimi, M.;Asemi, Z. Probiotic and selenium co-supplementation, and the effects on clinical, metabolic and genetic status in Alzheimer’s disease: A randomized, double-blind, controlled trial. Clin. Nutr. 2019, 38, 2569–2575.
Kaur, H.; Nagamoto-Combs, K.; Combs, C.K. Impact of modulating gut bacteria using antibiotic, probiotic, and prebiotic interventions in the APP NL-G-F mouse model of Alzheimer disease. Alzheimers Dement. 2020, 16, 42122
BoonWong,C.;Kobayashi,Y.;Xiao,J.ProbioticsforPreventingCognitiveImpairmentinAlzheimer’sDisease.InGutMicrobiota-Brain Axis; IntechOpen: London, UK, 2018; ISBN 978-1-78984-815-1
Kwoji ID, Aiyegoro OA, Okpeku M, Adeleke MA. Multi-Strain Probiotics: Synergy among Isolates Enhances Biological Activities. Biology (Basel). 2021 Apr 13;10(4):322. doi: 10.3390/biology10040322. PMID: 33924344; PMCID: PMC8070017.
Grumet L, Tromp Y, Stiegelbauer V. The Development of High-Quality Multispecies Probiotic Formulations: From Bench to Market. Nutrients. 2020 Aug 15;12(8):2453. doi: 10.3390/nu12082453. PMID: 32824147; PMCID: PMC7468868Bagga D, Aigner CS, Reichert JL, Cecchetto C, Fischmeister FPS, Holzer P, Moissl-Eichinger C, Schöpf V. Influence of 4-week multi-strain probiotic administration on resting-state functional connectivity in healthy volunteers. Eur J Nutr. 2019 Aug;58(5):1821-1827. doi: 10.1007/s00394-018-1732-z. Epub 2018 May 30. PMID: 29850990; PMCID: PMC6647073
Bagga D, Aigner CS, Reichert JL, Cecchetto C, Fischmeister FPS, Holzer P, Moissl-Eichinger C, Schöpf V. Influence of 4-week multi-strain probiotic administration on resting-state functional connectivity in healthy volunteers. Eur J Nutr. 2019 Aug;58(5):1821-1827. doi: 10.1007/s00394-018-1732-z. Epub 2018 May 30. PMID: 29850990; PMCID: PMC664707
Bagga D, Reichert JL, Koschutnig K, Aigner CS, Holzer P, Koskinen K, Moissl-Eichinger C, Schöpf V. Probiotics drive gut microbiome triggering emotional brain signatures. Gut Microbes. 2018 Nov 2;9(6):486-496. doi: 10.1080/19490976.2018.1460015. Epub 2018 Jun 14. PMID: 29723105; PMCID: PMC6287679.
Schlegel P, Novotny M, Klimova B, Valis M. "Muscle-Gut-Brain Axis": Can Physical Activity Help Patients with Alzheimer's Disease Due to Microbiome Modulation? J Alzheimers Dis. 2019;71(3):861-878. doi: 10.3233/JAD-190460. PMID: 31476155.
Mayo Clinic, Alzeimer’s Disease: Can Exercise Help Prevent Memory Loss?.




