Genetics
Mothers, Madness, and Mitochondria
Mitochondrial genes fit predictions of the imprinted brain theory.
Posted August 6, 2016
In a recent post, I reported my experience of psychosis thanks to a transient post-operative delirium. As I described, by far the most exhausting and arduous symptom was that of fits of compulsive cogitation, which made me analyse any and everything into having four different parts in excruciating exactitude and damnable detail. As I pointed out, this was self-evidently hyper-mentalistic, and forced me to run my brain at full power, leaving me totally exhausted and thankful for any respite.
Although only 2% of body weight, the brain consumes 20% of the available oxygen and glucose, and even more in childhood. At birth the brain represents 10% of total weight but consumes up to 65% of the body’s energy, while only 8% of an infant’s total metabolic rate is devoted to muscle tissue. In the first year and a half of life a human infant needs almost 10% more energy per day to run its brain than a chimpanzee of the same size. At 6 years of age the brain’s consumption of total oxygen intake peaks at about 50%. If you replaced the brain with a light bulb, it would be rated at just under 15 watts (the wattage of a refrigerator light). The ever-beating heart, by comparison, would radiate at 10 watts, and the skin would barely glow at one and a half. Energy consumption always produces heat as a by-product, and the human head has been engineered by evolution to radiate away as much of it as possible through a complex system of veins and an ability to sweat profusely. This explains why you sweat much more from your head and neck than anywhere else despite the fact that most of the body’s mass is concentrated in the trunk.
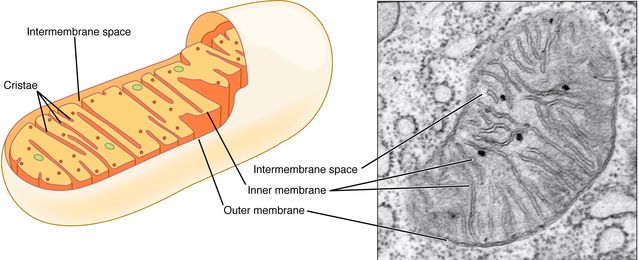
With these facts in mind, I can make a further comment that is highly pertinent to the imprinted brain theory. The crucial point is that energy is released in cells by mitochondria (above). These are tiny cells-within-cells, and are closely related to the typhus bacterium, Rickettsia prowazekii. Indeed, according to a widely accepted hypothesis, they originated when a larger cell incorporated a bacterium of this kind as a permanent, symbiotic resident.
Mitochondria provide the host cell with energy, somewhat as batteries do to machines. Unlike all other cell components, but again like bacteria (and despite having most of their genes located in the nucleus) mitochondria have their own, independent genome, comprising 37 genes on a single, circular DNA strand. And again like unicellular organisms such as the typhus bacterium, mitochondria are unisexual clones: normally a person’s mitochondria are exclusively derived from the mother’s egg cell, not from the father’s sperm. In fact, any paternal mitochondria that do make it into the fertilized egg cell are marked as such and duly eliminated. And contrary to what you might imagine, given the sperm’s vigorous activity compared to the egg’s relative passivity, the egg contains about a hundred thousand mitochondria, whereas the sperm has fewer than a hundred.
Mitochondrial diseases typically affect metabolically active tissues such as the muscles, brain, and the nervous system, resulting in seizures, movement disorders, blindness, deafness, and muscular degeneration. Mitochondria are enriched in the synapses of neurons, and are targeted towards active synapses. According to one account, “mitochondria have many mysterious properties, and can even form branching networks, communicating among themselves,” somewhat as neurons do.
A review of the literature published in 2015 remarked that comorbidity of mitochondrial dysfunction and psychiatric disorders is well established, even if the causal connection between them is not well understood. Mitochondrial factors in mental illnesses could be causative, coincidental, or consequential, and evidence for all three exists. Indeed, “it is possible that at least in some cases, mitochondria-related alterations observed in psychiatric patients are an epiphenomenon, related to disease-induced lifestyle and behavior, rather than a primary etiological factor involved in disease initiation and progression.”

Where debilitating diseases such as Alzheimer’s are concerned, loss of brain power related to mitochondrial morbidity is not surprising. Much the same might be said for autism spectrum disorder (ASD) seen as the result of deficits in mentalistic cognition. Indeed, this would explain why “accumulating clinical, genetic, and biochemical evidence suggests that mitochondrial dysfunction in ASD is more commonly seen than expected,” and why “Some patients with ASD phenotypes clearly have genetic-based primary mitochondrial disease.” (Quotes and figure left courtesy Richard H. Haas)
Nevertheless, the imprinted brain theory raises the contrary possibility that mitochondrial genes might be implicated in gain-of-function disorders as well: notably the hyper-mentalistic, positive symptoms of psychosis. Furthermore, the 2015 review from which I quoted above cites evidence of up-regulation of mitochondrial complex I subunits in the blood of schizophrenics; while the nuclear gene for mitochondrial DNA replication, POLG, has been reported to be significantly up-regulated in the frontal cortex of bipolar subjects.
Even more to the point where the imprinted brain theory is concerned, mitochondrial genes’ unisexual, maternal mode of inheritance means that you would expect them to be subject to selection with a bias in favour of the mother, and so to this extent, mitochondrial genes resemble maternally-active imprinted ones and indeed X chromosome ones. According to the imprinted brain theory, this leads to the prediction that enhanced expression of mitochondrial genes might be implicated in psychotic spectrum disorders and that reduced expression might similarly be implicated in autism spectrum ones, and as we have just seen, evidence for both already exists.
Besides being critically concerned with energy metabolism, mitochondrial genes are also now known to be implicated in so-called apoptosis, or programmed cell death: cellular suicide, if you like. This describes a genetically controlled, safe shutdown of cell function that does not harm surrounding tissues and leaves the dead cell suitably packaged for disposal by scavenger cells. Apoptosis is normally triggered whenever a cell is compromised, for example by becoming infected or pre-cancerous, and cancer is effectively the result of failure in this respect.
Given that risk of cancer is, as predicted by the imprinted brain theory, higher in autistics and lower in psychotics, a clear link with the maternal, mitochondrial genome is possible—particularly in view of the fact that many maternal, growth-restricting genes are also known to function as tumour-suppressors. Indeed, failure of apoptosis in the cells affected may also explain why autistics have a 100 to 190-fold increased risk of neurofibromatosis (benign nerve tumours) compared to the general population. And as we have already seen, the fact that any and all forms of hyper-mentalizing—and not just the compulsive thinking from which I suffered—probably demand increased energy output in the brain suggests that the maternal, mitochondrial genome may be intimately bound up, not only with apoptosis and cancer-suppression, but with hyper-mentalism in a way uniquely predicted by the imprinted brain theory.
(With thanks and acknowledgement to Richard H. Haas.)




