Placebo
The Quicksand of Self-deception: The Nocebo Effect
Giving patients too much information about potential harm may be harmful itself
Posted July 23, 2015

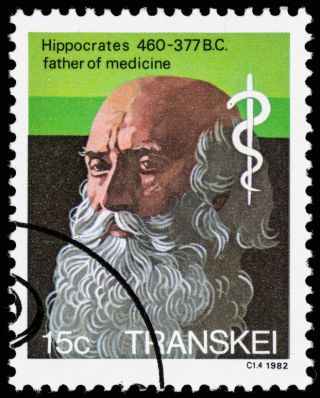
One of the first tenets of medicine “Do no harm,” originates from Hippocrates’s treatise Epidemics (section XI)—“as to diseases, make a habit of two things: to help or at least do no harm.” It is also the title that neurosurgeon Henry Marsh chose for his extraordinary recently published memoir. There are times, though, when physicians can, perhaps inadvertently, cause more harm than good when they reveal all the potential side effects of a medication or therapeutic intervention, including those related to treatments for excessive weight and weight-related disorders.
There are many factors involved in the psychology of administering a medication or prescribing a treatment, including the quality of the physician-patient relationship itself, what doctors and patients believe about the particular treatment and how it works, what they each expect to happen, or specifically with a medication, the medication’s physical attributes such as its color, shape, smell, method of administration, or even its name.
From the Latin “nocebo,”—“I will harm,” the nocebo reaction (also called the nocebo “effect,” “response,” or “phenomenon”), was first described as the “contrary effect” to the placebo response by Walter P. Kennedy (1961, Medical World.) Kennedy described what he called the “unoriginal observation” that many of the subjects in his clinical trials exhibited non-specific adverse reactions. Kennedy noted that every physician “has met the nocebo reaction, even if he has not labelled it as such….” It has been described as placebo’s “mirror image” (Cohen, Bioethics, 2014) or its “evil twin” (Schedlowski et al, Pharmacological Reviews, 2015.)
The nocebo reaction is a form of self-deception that involves the self-fulfilling prophecy. In other words, “People perceive what they expect to perceive.” (Wells and Kaptchuk, American Journal of Bioethics, 2012) Many writers, as diverse as the Ancient Greek orator Demosthenes (3rd Olynthiac) and the American statesman and writer Benjamin Franklin (Poor Richard’s Almanack), have recognized how easily we are able to deceive ourselves. Robert K. Merton (The Antioch Review, 1948), described the “self-fulfilling prophecy” as involving “fears that are translated into reality” and noted that its “specious reality…. perpetuates a reign of error.” In fact, nocebo reactions can have far-reaching consequences: they can lead to “epidemic waves” of reports of adverse events and drugs being removed prematurely from market as well as a patient’s psychological distress and even noncompliance with treatment. (Wells and Kaptchuk, 2012) Even reported complications observed when switching from a brand name medication to the generic can be related to nocebo responses. (Schedlowski et al, 2015)
The nocebo concept, though, suffers from a lack of a clear and precise standardized research definition. For Barsky et al (JAMA, 2002), nocebo responses describe negative treatment effects that are not directly attributable to a drug’s pharmacokinetics. These nonspecific side effects are often “idiosyncratic and not dose-dependent.” They are what Barsky et al call “misattributions” by the patient.
Schedlowski et al (2015) define two variants: new or worsening of symptoms associated with a pharmacologically active drug, but also reduced efficacy due to negative expectations or prior experiences. Some researchers, as described by Symon et al (J. Advances in Nursing, 2015) include negative side effects that can also occur when a patient is given an actual placebo, i.e. a totally pharmacologically inert or harmless substance or therapy that is not expected to have either beneficial or harmful effects. Others define a nocebo effect generally when a treatment “expected to have beneficial effect has a detrimental outcome.” (Dodd et al, Journal of Clinical Psychiatry, 2015) Jakovljevic (European Neuropsychopharmcology, 2014) notes that nocebo responses are “multifactorial, multidimensional, and etiologically complex,” and researchers cannot even agree on whether these responses are either “the effect of” or “response to.”
The prevalence of nocebo effects varies, depending on the intervention being prescribed or the condition being treated. Symon et al (2015) found a general prevalence internationally of 3 to 27% in a review of 48 empirical studies. More specifically, in a study of treatment for major depression, Dodd et al (2015) found that nocebo effects may explain almost 64% of treatment-emergent adverse effects and almost 5% of discontinuation in a large placebo-treated patient sample of over 2400 subjects.
Meynen et al (American Journal Bioethics, 2012) maintain that the nocebo effect “shows us that mere information about potential harm is likely to be harmful itself.” Says Meynen et al, “The physician’s words not only describe reality, but they modify and create reality.” These researchers, though, emphasize that, with the advent of the internet, the “treating physician is no longer the gatekeeper of medical information” with the result that patients can (and do) retrieve information about their treatments from many sources.
Little is known about the predictors of nocebo responses. ((Schedlowski et al, 2015) Barsky et al (2002) report that those patients who expect to have distressing side effects—i.e. negative expectation— are more apt to develop them. These responses occur more often in women (unlike placebo reactions that apparently occur equally in men and women) (Dodd et al, 2015). Psychological symptoms, such as depression and anxiety may make certain patients more prone to nocebo responses, as well as those with a type A personality (e.g. those competitive, with a sense of urgency and a tendency to hostility) or a pessimistic nature.
The mechanisms for nocebo reactions also remain poorly understood, but may involve conditioned learning and expectancy. For example, patients previously treated with chemotherapy can develop a conditioned nausea response just by seeing the nurse or entering the treatment room even before receiving another treatment. Allergic reactions have occurred in patients expecting to receive an allergen but receiving only saline. Further, nocebo reactions have been associated with dopamine, the endogenous opioid system, and cholecystokinin, and studies involving neuroimaging have shown that the “mere expectation of symptoms can activate brain structures.” (Schedlowski et al, 2015)
Several sources, including Cohen, 2014, focus on medical ethical issues involved with the nocebo reaction, primarily the conflict between respecting a patient’s autonomy and the principle of nonmaleficence, i.e., “do no harm.” (Wells and Kaptchuk, 2012) In other words, if disclosing detailed potential side effects or complications of a treatment can cause harm or adverse effects in a patient, should a physician give full disclosure, if that is even possible? On the other hand, failure to disclose possible effects can be seen as paternalism. And hence there exists what these researchers call an inherent “ethical conundrum.”
Bottom line: Factors contributing to the nocebo effect remain “elusive and are inherently difficult to profile and characterize.” (Dodd et al, 2015) Patients can become mired in the quicksand of self-deception when burdened with too much clinical information that becomes self-fulfilling. Both physicians and patients should not assume that reported troublesome side effects necessarily stem from the pharmacological effects of a particular medication or intervention, especially when the symptoms are vague or when a patient is particularly anxious. Physicians must be sensitive to creating an optimal balance between respecting a patient’s autonomy as evident in offering full disclosure of information and unnecessarily fostering an environment of paternalism, in the interest of protecting a patient from harm, by withholding it.
Note: Scholars of Shakespeare will know that my title derives from Henry VI, part 3 (Act V, scene 4. 26): “What Clarence but a quicksand of deceit?”