Depression
The Melancholy of Anatomy: Excessive Weight and Depression
The complex relationship between weight and depressive disorders
Posted May 21, 2015 Reviewed by Hara Estroff Marano
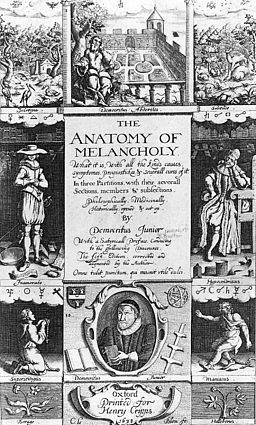
The Oxford scholar Robert Burton published his 2000-page treatise The Anatomy of Melancholy in the early 17th century. The book has been described as encyclopedic—an extraordinary combination of self-help book and medical textbook. Burton worked and reworked his tome, with multiple editions throughout his life, as a therapeutic means of dealing with his own melancholia.
He defined “melancholia” as a mind anguished by “fear and sorrow.” “Melancholy,” from the Greek words for “black bile” refers to the ancient theory of Hippocrates whereby an imbalance of one of the four humors (black bile, yellow bile, phlegm, and blood) was believed to result in disease. For Burton, melancholia was a disease that affected mind, body, and soul and had many causes, including “bad diet,” either in “substance” or “quantity.”
Fast forward to our current psychiatric nomenclature, the DSM-5. Depression, of course, can be a transient symptom but the “depressive disorders” are defined by the “presence of a sad, irritable or empty mood, accompanied by somatic and cognitive changes that significantly affect” a person’s functioning. There are several categories differentiated by “duration, timing, and presumed etiology.”
We now use the specifier term “with melancholic features” to include particularly severe symptoms: “profound despondency and despair,” marked agitation or psychomotor retardation, feeling worse in the morning, early morning awakening, excessive guilt, and loss of appetite with weight loss. Ironically, depression, though, can also be associated with weight gain. This is seen in so-called “atypical depressions,” with the symptom cluster that includes “mood reactivity” (i.e. ability to be cheered up at least temporarily when presented with positive events), significant weight gain or increase in appetite, increased sleep (i.e. “hypersomnia”), “leaden paralysis,” (e.g. heavy feeling in arms and legs) and particular sensitivity to rejection that affects someone socially and occupationally.

Does a depressive disorder lead to weight gain or does weight gain lead to a depressive disorder? Studies over the years have been confusing, inconsistent, and even contradictory. Psychiatrist Albert Stunkard, one of the pioneers in obesity research, and his colleagues (1998, International Journal of Obesity) noted that it should not be surprising that those who are weight-challenged would have psychological difficulties, including depression, because of the prejudice and overt discrimination to which these people are often subjected. But early researchers, including Stunkard, could not find “psychological characteristics” or a specific “distinctive personality” in those who were obese that could “consistently distinguish them” from those who were not.
What these researchers found, though, is that those with excessive weight who sought treatment were more likely to suffer from depression and/or anxiety. More recent research (Preiss et al, Obesity Reviews, 2013) has focused on risk factors associated with comorbid obesity and depression and possible causal relationships, and found more consistent associations between them in their systematic review of 46 studies.
Preiss et al found, however, considerable differences in study methodologies, population characteristics, means of defining and even measuring depression, and even inconsistent reporting of results across the studies. Key factors associated with this relationship included the severity of obesity, particularly when a person’s body mass index (BMI) is above 40 kg/m2 (Class III obesity); socioeconomic status; body image, physical health, disordered eating (e.g. binge eating), and experience of stigma. For example, those in a higher socioeconomic class who are obese experience significant prejudice and discrimination that may lead to developing depression. Further, body image dissatisfaction may be an important risk factor and important target of treatment interventions.

Luppino et al (Archives of General Psychiatry, 2010) performed a systematic review and the first meta-analysis of longitudinal studies of 15 studies, including over 55,000 subjects. These researchers found “bidirectional associations” between obesity and depression: obese persons had a 55% increased risk of developing depression over time, whereas depressed persons had a 58% risk of becoming obese, with the association between obesity and depression stronger than overweight and depression, indicating a so-called “dose-response” association. Their longitudinal meta-analysis confirms this reciprocal relationship for both men and women, with follow-up as long as 28 years in one study.
In other words, obesity increases the risk of depression and prior depression increasing the likelihood of obesity. (Lopresti et al, Progress in Neuro-Psychopharmacology & Biological Psychiatry, 2013.) Rather than thinking of the two conditions as comorbid, researchers like Mansur and his colleagues (Neuroscience and Biobehavioral Reviews, 2015) think of a “bidirectional convergent relationship.”Allison and his colleagues, though, caution (American Journal of Preventive Medicine, 2009), “Obesity and depression clearly coexist, but the available data do not unequivocally demonstrate a causal relationship between the two.”
What researchers have also found is that obesity can negatively impact treatment outcomes in mood disorders and those with depression often do less favorably with weight loss interventions: they tend to lose less weight and have more difficulty with long-term maintenance of any weight lost. The fact that depression causes an increase in weight may be due to neuroendocrine disturbances, (e.g. activation of the hypothalamus pituitary adrenal—HPA— axis and increased cortisol production), adoption of unhealthy lifestyle (e.g. lack of sufficient exercise), and use of anti-depressant medications (particularly paroxetine, mirtazapine, and amitriptyline). Because weight gain may be a late consequence of depression, weight should be monitored in those with depressive disorders; furthermore, mood should be monitored with overweight or obese patients. (Luppino et al 2010)
Rossetti (Frontiers in Psychology, 2014) and her colleagues have suggested that the hormone leptin produced by adipose tissue “may represent a biological substrate underlying the pathogenesis of both obesity and depression.” There is evidence that “impaired leptin signaling cascades” may be the biological mechanism that links obesity and depression, particularly when obesity is paired with compulsive overeating. Some researchers even describe a “metabolic mood disorder” (e.g. a predominantly depressive illness with an overrepresentation of atypical features, anxiety, and a chronic course.) (Mansur et al, 2015)
Bottom line: The relationship between obesity and depression is complex. Both disorders are heterogeneous with “overlapping pathologies” (Rossetti et al, 2014) and significant contributions from both genetic and environmental factors. Says Mansur et al (2015) “Considering the high impact of obesity and mood disorders in disability and morbidity, the co-occurrence of these conditions is incredibly relevant from a public health perspective.” Clearly, there is need for further research to determine all the mechanisms involved especially because of the possible cumulative public health burden from both.





