Vagus Nerve
Vagus Nerve Stimulation May Ease Emotional and Physical Pain
Noninvasive vagus nerve stimulation (nVNS) may dampen pain associated with PTSD.
Posted February 13, 2019
Researchers at the University of California San Diego School of Medicine are testing a novel bioelectronic intervention called "noninvasive vagus nerve stimulation (nVNS)" to address various types of pain and mental health issues associated with post-traumatic stress disorder (PTSD). The findings of this multi-faceted pilot study, "Noninvasive Vagus Nerve Stimulation Alters Neural Response and Physiological Autonomic Tone to Noxious Thermal Challenge," were published February 13 in the journal PLOS ONE.
This exploratory research was spearheaded by Imanuel Lerman, an associate professor at the UCSD School of Medicine and a pain management specialist at UC San Diego Health. Lerman is also affiliated with the Veterans Affairs San Diego Healthcare System.
Lerman's objective with this randomized, controlled study was to investigate how noninvasive vagus nerve stimulation influences the way someone experiences both physical and emotional pain—with the hope of someday using nVNS to help veterans with PTSD.
Although the sample size of this study was small, Lerman and colleagues found that participants who were pre-treated with noninvasive vagus nerve stimulation experienced lower perceptions of pain from a heat stimulus (i.e., noxious thermal challenge) applied to the leg in comparison to a control group that did not receive nVNS.
"It's thought that people with certain differences in how their bodies—their autonomic and sympathetic nervous systems—process pain may be more susceptible to PTSD," Lerman said in a statement. "And so we wanted to know if we might be able to re-write this 'mis-firing' as a means to manage pain, especially for people with PTSD."
Lerman co-led this study with senior author Alan Simmons, who is director of the fMRI Research Laboratory at Veterans Affairs San Diego Healthcare System and an associate professor of psychiatry at UC San Diego School of Medicine.
What's the Difference Between Vagus Nerve Stimulation (VNS) and nVNS?
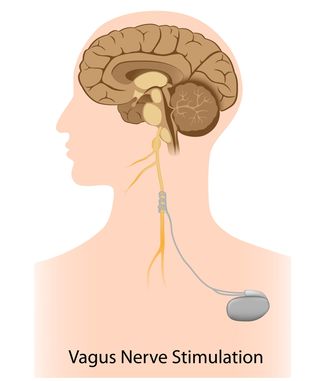
Since the 1990s, doctors have been using small, matchbook-size surgically implanted vagus nerve stimulation (VNS) devices to reduce the frequency and severity of seizures in epilepsy patients who don’t respond to medications. Traditional VNS requires an outpatient surgical procedure (which usually takes under an hour) to implant a pacemaker-like stimulating device under the skin near the collarbone and attach it to a branch of the vagus nerve.
In May of 2000, vagus nerve thought leader and research pioneer Kevin J. Tracey and colleagues published a landmark paper (Borovikova et al., 2000) on VNS in the journal Nature. Two years later, this was followed by another seminal paper in Nature, "The Inflammatory Reflex" (Tracey, 2002).
In 2016, Tracey published another groundbreaking follow-up paper, "Vagus Nerve Stimulation Inhibits Cytokine Production and Attenuates Disease Severity in Rheumatoid Arthritis," (Koopman et al., 2016) in PNAS. (See "Vagus Nerve Stimulation Dramatically Reduces Inflammation")
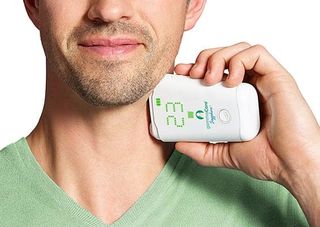
With a typical nVNS device, you simply press a smartphone-size gadget against the side of your neck and self-administer a prescribed dosage of electrical vagus nerve stimulation that is delivered through the skin.
In 2017, the FDA first approved the use of any noninvasive vagus nerve stimulation (nVNS) for the treatment of acute pain associated with cluster headaches. In January of 2018, the FDA approved the use of nVNS to treat episodic migraine pain.
To the best of my knowledge, gammaCore (electroCore LLC) is the only company currently manufacturing a hand-held noninvasive vagus nerve stimulation device. (For the record: I have no conflict of interest related to gammaCore/electroCore LLC or any incentive to promote their products.)
Noninvasive Vagus Nerve Stimulation May Help Dampen Physical and Emotional Pain
In their latest fMRI-based study (Lerman-Simmons et al., 2019) on the possible abilities of nVNS to dampen the sensation of physical and emotional pain, the researchers made three key discoveries:
1. The fMRI neuroimaging results showed that nVNS reduced peak response to scorching-hot heat stimulus in brain areas involved in sensory and discriminative pain processing, as well as brain areas referred to as so-called “emotional pain centers.” Interestingly, if someone was pre-treated with noninvasive vagus nerve stimulation, these pain-related brain regions “lit up” in the fMRI ten seconds later than in participants who received sham-nVNS treatment.
2. Noninvasive vagus nerve stimulation altered how the autonomic nervous system responded to heat stimulus based on sweat measurements. For example, in participants who were pre-treated with nVNS, sweat response decreased over time. Conversely, sweat response to heat stimulus increased in the sham-treatment group.
3. Brainstem centers that drive fight-or-flight stress responses—and also control the secretion of sweat in response to pain—appear to be dampened by noninvasive vagus nerve stimulation.
"Not everyone is the same—some people may need more vagus nerve stimulation than others to achieve the same outcomes and the necessary frequencies might change over time—so we'll need to personalize this approach," Lerman emphasized in a statement. "But we are hopeful and looking forward to the next steps in moving this approach toward the clinic."
The authors acknowledge that this first-of-its-kind research has important limitations such as being a pilot study and having a small sample size. Therefore, these findings may not adequately represent those of a larger population and should be considered preliminary. More research is needed.
The next phase of research on noninvasive vagus nerve stimulation being conducted by Lerman and colleagues will involve military veterans both with and without PTSD symptoms. This clinical trial will take place in San Diego and is being funded by the Veterans Affairs Healthcare System. The goal of this upcoming study is to determine if at-home nVNS can reduce both the emotional pain and neural inflammation associated with PTSD.
If you, or someone you know, is a veteran who might be interested in participating in this clinical trial (being launched in 2019) please email achiu@vapop.ucsd.edu or call 858-552-8585.
Over the years, I've written extensively about everyday ways to engage the vagus nerve and improve vagal tone holistically. For more, see my nine-part series "A Vagus Nerve Survival Guide to Combat Fight-or-Flight Urges," "Vagus Nerve Facilitates Guts, Wits, and Grace Under Pressure," and "Self-Compassion Calms and Soothes Fight-or-Flight Responses."
References
Imanuel Lerman, Bryan Davis, Mingxiong Huang, Charles Huang, Linda Sorkin, James Proudfoot, Edward Zhong, Donald Kimball, Ramesh Rao, Bruce Simon, Andrea Spadoni, Irina Strigo, Dewleen G. Baker, Alan N. Simmons. "Noninvasive Vagus Nerve Stimulation Alters Neural Response and Physiological Autonomic Tone to Noxious Thermal Challenge." PLOS ONE (First Published: February 13, 2019) DOI: 10.1371/journal.pone.0201212




