Depression
Untreated Depression Linked to Telomeres, Aging, and Disease
Scientists unravel the biological ripple effect of chronic depression.
Posted May 24, 2013

Telomeres in pink
Untreated depression creates biological changes that accelerate aging and increase the risk of life-threatening diseases. Major Depressive Disorder (MDD) can trigger changes in immune cell function and the length of telomeres.
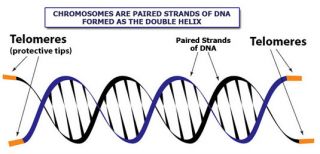
Telomeres are tiny units of DNA-protein that seal off and protect the ends of chromosomes and act as a biological clock to control a cell's life. Over time, untreated depression can shorten telomeres and make people prone to diseases typically associated with advanced age such as heart disease, diabetes, osteoporosis, and stroke.
A team led by Owen Wolkowitz, MD, professor of psychiatry at UC San Francisco (UCSF) have been studying the biological link between chronic depression and an enzyme called telomerase. The scientists discovered that within the cells of the immune system, activity of telomerase is greater, on average, in untreated individuals with major depression. These findings were presented at the annual meeting of the American Psychiatric Association in San Francisco on May 22, 2013.
Telomerase and Telomeres
Telomerase is an enzyme that lengthens protective end caps on the chromosomes' DNA, called telomeres. Shortened telomeres have been associated with chronic diseases and premature death in previous studies by Wolkowitz and colleagues at UCSF. Wolkowitz believes that the elevated telomerase activity in untreated major depression could represent the body's attempt to combat the progression of disease, in order to prevent biological damage in long-depressed individuals.
There seems to be a paradoxical hyperactive increase of telomerase in untreated depressed individuals which indicates that their bodies are attempting to overcompensate for telomere damage caused by chronic depression. Healthy increases of telomerase during treatment, however, may represent true improvement in depression.
"We speculate that telomerase may provide a biological marker for antidepressant responses," Wolkowitz said. "Once we better understand these systems, we will be in a stronger position to treat depression and possibly prevent some of its associated physical illnesses."
The researchers measured telomere length in the same immune cells. “Only very chronically depressed individuals showed telomere shortening,” Wolkowitz said. "The longer people had been depressed, the shorter their telomeres were," he said. "Shortened telomere length has been previously demonstrated in major depression in most, but not all, studies that have examined it. The duration of depression may be a critical factor.”
Telomerase and the Hippocampus
The researchers also made a surprising discovery that telomerase may play a role in stimulating neurogenesis (new cell growth) in the hippocampus—a brain structure critical for learning and memory.
Using magnetic resonance imaging (MRI), the UCSF researchers found that in untreated depressed participants, the size of the hippocampus was associated with the amount of telomerase activity in white blood cells. “Such an association at a single point in time cannot be used to conclude that there is a cause-and-effect relationship with telomerase helping to protect the hippocampus, but it is plausible,” Wolkowitz said.
The researchers found that the telomerase enzyme's activity went up when some patients began taking an antidepressant. In fact, depressed participants with lower telomerase activity at baseline—as well as those in whom enzyme activity increased the most with treatment—were the most likely to become less depressed with treatment.
"Our results are consistent with the beneficial effect of telomerase when it is boosted in animal studies, where it has been associated with the growth of new nerve cells in the hippocampus and with antidepressant-like effects, evidenced by increased exploratory behavior," Wolkowitz said.
Conclusion
"While this finding itself might seem depressing, there is yet good news: many lifestyle factors like exercise and aspects of diet have been linked to longer telomeres," said Elissa Epel, PhD, an associate professor in the UCSF Department of Psychiatry and co-author of studies on telomeres. "So while our personal history matters, it is possible that what we do today may matter even more, in terms of protecting our telomeres."
Wolkowitz's team also studies chronic inflammation and the biochemical phenomenon of oxidative stress, which he said have often been reported in major depression. Wolkowitz is exploring the hypothesis that inflammation and oxidative stress play a role in telomere shortening and accelerated aging in depression. For more on lifestyle changes that can reduce the risks of chronic inflammation please check out my Psychology Today Blog “The Life Threatening Toll of Stress.”
Wolkowitz cautions that the new findings are preliminary due to the small size of the study and must be confirmed through further research. The study included only 20 depressed participants who had been untreated for at least six weeks and had an average lifetime duration of depression of about 13 years.
As a next step, UCSF researchers plan to replicate these preliminary findings in a larger sample of depressed individuals in order to explain why certain people develop shortened telomeres and physical disease, and how that process can be combated.




