Health
Australian Short Course Award Addresses Public Mental Health
Fostering development by enhancing mental health in Africa.
Posted June 17, 2019
The Australian Government’s Department of Foreign Affairs and Trade funds Australia Awards short courses, some of which are directed at the development needs of countries in Africa. In a new initiative, the short course awards in 2019 will provide training in mental health care in a public health context.
Queensland University of Technology, in collaboration with colleagues from Melbourne University and Stellenbosch University in South Africa, will oversee the delivery of the course, with participants drawn from a range of countries in Africa. Participants are required to work in the area of mental health and be in a position to translate their learning into improved practices. The program will be repeated over the coming years, with a view to building capacity in various parts of Africa, and thus contribute to the improvement of mental health services across the continent.
The program is designed to introduce participants to best practice in promoting mental health, taking into account local cultural contexts and knowledge. The program will address prevention, early intervention, and clinical skills as they relate to the assessment and general management of mental health conditions.

For the next several blog posts, I will focus on Global Mental Health in Africa and provide updates on the program we are running. In this blog, I will outline some background to the definition of mental health within a global health context and point to some of the influences which have informed the development of the project.
Mental health has been defined by the World Health Organisation (WHO) as referring to a state of well-being and facilitating the capacity of all people to realize their own potential, to cope with the normal stresses of life, to work productively and fruitfully, and to contribute to their respective communities. The WHO stresses the positive dimensions of mental health in its constitution: "Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity". This definition is important in acknowledging that mental health is more than the absence of mental disorders; that is, there is no health without mental health.
The goal of global mental health is to address health inequities internationally. Within this context, it is recognised that mental health is determined by a range of cultural, socioeconomic, environmental, and biological influences. Factors operating at each of these levels serve to influence the ways in which people, whether individually or collectively, think, feel, and relate to and interact with one another, as people seek to lead meaningful lives within larger communities and contribute to society.
Contributing to global mental health cannot be limited to the more traditional domains of identifying, assessing, and treating people who are deemed to suffer from mental health problems as defined within the dominant Western perspective. Transcultural psychiatrists and medical anthropologists refer to the importance of taking both emic (perspective of the person) and etic (from an outside perspective) factors into account. Not surprisingly, there is a diversity of views that influence the ways in which global mental health is conceptualized. In this blog, I wish to simply make reference to two views, which represent the bias of each approach.
At one end of the continuum, psychiatrist Vikram Patel heads the Centre for Global Mental Health, which aims to close the treatment gap for people living with mental, neurological, and substance use disorders in low resource countries through program development, training, and designated projects. The centre has played a key role in advocacy, training health workers internationally, including suicide prevention, psychological first aid, and group therapeutic approaches to the treatment of depression as examples.
Professor Patel has been enormously productive in providing relevant literature related to global mental health initiatives. This literature is largely within the public domain. The centre has also produced important guidelines to address a range of topics such as reducing stigma, and a range of mental health-related training videos. Patel and colleagues have highlighted the burden and impact of untreated mental disorders and provided an argument for a global approach to redress disparities between services available in high-income countries such as Australia and those in low-income countries across the African continent (Global Mental Health Group, 2007).
The global burden of mental, neurological and substance use (MNS) disorders for low and middle-income countries is estimated for unipolar depressive disorders, measured in terms of disability-adjusted life years (DALY), to equate to 55.5 (DALY); for alcohol use disorders 19.5 (DALY), and for schizophrenia 15.2 (DALY).
In contrast, there is an argument that the Global Mental Health movement is simply applying “Western” psychiatric categories, concepts and interventions to people, with little regard to local idioms of distress, or respecting more traditional knowledge and understanding. In their critique of Global Mental Health, writers such as Fernando and Summerfield argue that the biological determinism underpinning such approaches have the unintended consequences of medicalizing everyday distress and serve the economic agenda of the pharmaceutical industry.
These theorists refer to Global Mental Health as a new form of ‘neo-colonialism’ or ‘medical imperialism,’ arguing that the proponents are at risk of ignoring the cultural dimensions of mental illness, which leads to inappropriate diagnoses and fails to recognize local knowledge as expressed in indigenous healing systems, which are endemic in many more traditional African countries.
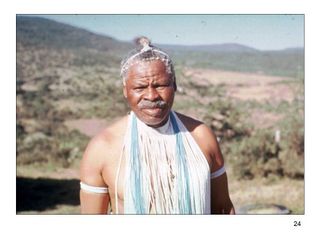
I have some firsthand experience as a young researcher working with indigenous healers in Southern Africa some years ago, and I was struck by the disparity of views by “the medical establishment” and insider knowledge.
In responding to people who may hear voices and see things which other people do not see, psychiatrists would invariably think of schizophrenia. The local community and indigenous healers (Amagqira) would likely refer to the person as suffering from an illness (thwasa) resulting from a calling by the ancestors for the person to undergo training and themselves become a healer. This understanding is consistent with the cosmology of the traditional members of the community.
These various perspectives raise important issues in addressing global mental health and the importance of considering context in the development of programs. There is clearly a need to take cognizance of those areas where Western approaches clearly have a contribution to make and to also consider local knowledge and beliefs where such belief systems contribute to a sense of meaning within communities. It is well to remember that “wellbeing and personal resilience are linked to social connectedness and the sense of a coherent world” (Summerfield 2008).
The current program is the result of consultation and clinical evidence in addressing the mental health needs of people in low-income countries. At the same time, the program will emphasize the values of gender equity and social inclusion as being fundamental to meaningful development of services in a contemporary health environment. Through the Australia Awards short course commencing this year, we will be drawing upon an array of resources, both in Australia and in Africa, to best address the needs of health workers at the coalface in the areas of service development and delivery.




