Gaslighting
When It's Not All in Your Head
How to deal with medical gaslighting.
Posted July 27, 2022 Reviewed by Gary Drevitch
Key points
- Cognitive bias in physicians can wrongly blame a patient's symptoms on psychological factors.
- Medical gaslighting disrupts accurate diagnoses of medical conditions, particularly rare illnesses.

I've worked with many children and adults who've been told to seek mental health treatment by medical professionals, because their physical complaints were not real. These patients were told things like, "It's all in your head," "There's nothing medically wrong," or"You're fine and have to learn how to deal with the pain."
In over 30 years of practice, all of these traumatized patients - the majority of them females - did, indeed, have real medical issues. They were not hypochondriacs, attention-seeking, or experiencing a conversion disorder or a somatic symptom disorder. They were dealing with rare illnesses that weren't considered plausible in the medical community.
My clinical assessment of their symptoms suggested that mental health issues were not causal. Working together, the patients and I insisted on further medical assessments, seeking specialists out of state, and even contacting universities and research centers to find experts. Some of the uncommon medical disorders finally diagnosed included Chronic Appendicitis, Ehlers-Danlos Syndrome, Chiari Malformations, Meniere's Disease, Cyclical Vomiting Syndrome, and Pheochromocytoma.
It was not all in their head.
Rare Diseases
Rare diseases are tricky things when you look at them individually. It's true that a specific rare disease may affect only a miniscule number of children and adults. However, the number of rare illnesses is quite large. According to The National Organization for Rare Disorders (NORD) there are more than 7,000 rare diseases, with studies showing in the United States alone, as many as 30 million people experiencing a rare disease in their lifetime. So when we talk about a rare disease, it may not really be that rare.
In medical school, doctors in training are taught to consider common diagnoses and not rare ones. This enduring approach, based on the principle of Occam's razor, holds that simple explanations are preferred over more complex ones. So even though 4% of the world population is affected by a rare illness at any given time, most medical professionals believe it's unlikely one will present in their consultation room. But studies suggest otherwise, and indicate most physicians will come face to face with a rare disease in their professional career.
Medical Gaslighting
Some health professionals thoughtfully regard chronic pain and symptoms seriously, recommending standard diagnostic tests and assessments to identify what's wrong and offer treatment. When doctors don't readily have a diagnosis for a pateint's complaints, there are a variety of things they may do. Sometimes, they'll revisit your patient history and list of symptoms to dig deeper. They may send you for more tests, or refer you to a specialist. But sometimes, the physician shifts to a diagnostic explanation that's more psychological than medical: that your mind is causing your symptoms. Sometimes they might be accurate in this assessment. Other times, it may be a missed opportunity for further specialized medical evaluation.
It's been my experience that some doctors approach this mind-stress possibility with great care, professionalism, and respect for the patient. But others venture down this mental health path with a different attitude - one that demeans, stigmatizes, minimizes, and even bullies the patient. This is called medical gaslighting, and it's a traumatizing experience for a patient:
"Stop Googling your symptoms."
"You just need to take a vacation."
"No more questions today. I have other patients to see."
As Canadian doctor Sarah Fraser, has written, "Gaslighting has been used by physicians to dismiss women’s health problems, enforcing the misogynist stereotype that women are irrational and hysterical, a prejudice that dates back centuries."
The Diagnostic Odyssey
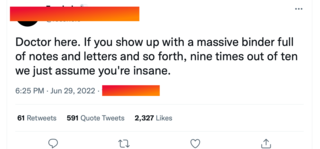
Most patients with undiagnosed rare illnesses have endured frustrating and discouraging visits with doctors. Often they come to appointments with self-created files containing tests and reports that document their diagnostic odyssey. Sometimes, physicians find this helpful. Other times, it's met with a stigmatizing response, as seen in a recent June 2022 Twitter feed about patients who come in with notes.
Research tells us that many cultural groups have higher rates of medical misdiagnosis and underdiagnosis because of implicit physician cognitive bias: children, people of color, LGBTQIA individuals, women, those who are obese, the homeless, the mentally ill, and the elderly all may experience this kind of medical gaslighting.
When patients have chronic pain and are faced with dismissive responses that imply they're mentally ill, it damages the entire health-care industry by causing medical mistrust.
5 Tips for Diagnosing Your Illness
When it comes to your physical and mental health, you have to be your own advocate. You need to create a team of health-care experts who make you feel heard, seen and valued. Together you can work toward the same goal: uncovering what has yet to be identified.
- Good primary care. Make sure you have a primary care physician who consistently listens to your needs. If you're feeling ignored or minimized, express your disappointment. If this is met with anything other than sensitivity, it's time to find another practitioner.
- Get a second opinion. Consider seeking a specialist to address your concerns. Studies show that 88% of patients looking for a second opinion will leave that appointment with a medical diagnosis or a new direction to pursue for further assessment of symptoms.
- Genetic testing. With over 7,000 known rare disorders - and more being discovered each year, according to the Genetic and Rare Diseases Information Center - consider accessing genetic testing for more precision in your diagnosis.
- Shrink it up. Welcome the addition of a mental health professional to your team. Working together, you can affirm your mental health is not the cause of your symptoms. And you can have a safe place to explore thoughts and feelings as you search for answers.
- Persist. Persist. Persist. Rare and uncommon disorders can take months and even years to diagnose. So be persistent and consistent in your diagnostic pursuit. And if there are moments when you're overwhelmed, ask others to help.




