Cognitive Behavioral Therapy
Cognitive Behavior Therapy for Adolescents With Eating Disorders
Enhanced CBT is a promising alternative for adolescents with eating disorders.
Posted July 25, 2024 Reviewed by Michelle Quirk
Key points
- CBT-E actively involves the young people in the treatment, and it is well accepted by patients and parents.
- The collaborative nature of CBT-E is particularly beneficial for ambivalent young patients.
- CBT-E accommodates parents who may not be able to participate in all treatment sessions.
Eating disorders can profoundly impact the psychosocial functioning and physical health of adolescents. Early and effective treatment is essential to prevent long-term adverse and devastating effects. The National Institute for Health and Care Excellence (NICE) recommends cognitive behavior therapy (CBT) for adolescent eating disorders when family therapy is unacceptable, contraindicated, or ineffective. This recommendation is based on promising results from an enhanced version of CBT (CBT-E), adapted for adolescents aged 12 to 19 with eating disorders.
Origin of CBT-E for Adolescents
CBT-E was initially developed for adults with eating disorders at the Centre for Research on Eating Disorders at Oxford (CREDO). The idea to adapt CBT-E for adolescents originated a decade ago at the Department of Eating and Weight Disorders of Villa Garda Hospital in Italy during periodic supervision by Professor Christopher Fairburn. Two main clinical observations prompted this project:
- Adolescents with eating disorders share the same specific psychopathology (e.g., overvaluation of weight and body shape, rigid dieting, excessive exercise, binge eating, and purging behaviors) as adults. They could benefit from CBT-E, a treatment designed to address this specific psychopathology.
- Adolescents, despite often being in a strongly egosyntonic phase of their eating disorder, can actively engage in individual psychological treatment.
Key Adaptations of CBT-E for Adolescents
CBT-E for adolescents incorporates three distinctive characteristics to accommodate young patients with eating disorders:
- Periodic medical evaluations and a lower threshold for hospitalization are integral, given the severe medical complications (e.g., osteopenia and osteoporosis) associated with eating disorders in this age group.
- Special efforts are made to engage adolescents in treatment and change, as they often do not recognize they have a problem.
- Parents are usually involved in treatment due to the age and circumstances of the patients.
Description of CBT-E for Adolescents
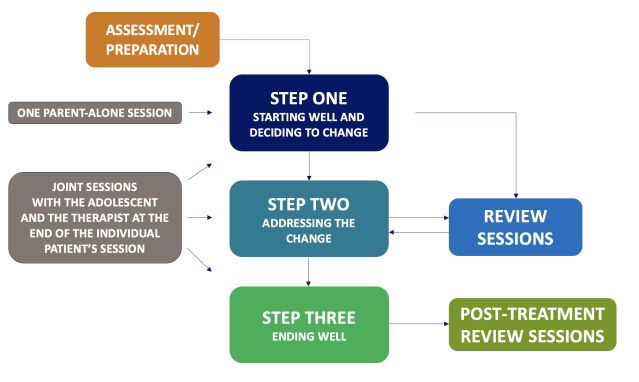
CBT-E for adolescents involves two assessment/preparation sessions, followed by three main steps, one or more review sessions, and three post-treatment review sessions (Figure). The treatment lasts about 20 weeks for non-underweight patients and about 30-40 weeks for underweight adolescents.
Parents participate in a 90-minute interview during the first week of treatment and in six to eight brief sessions (15-20 minutes) following the individual sessions with the patient.
General Treatment Strategy
After assessment, patients are educated on the disease model and the CBT-E psychological model for understanding eating disorders and the therapeutic approaches based on them (see Table).
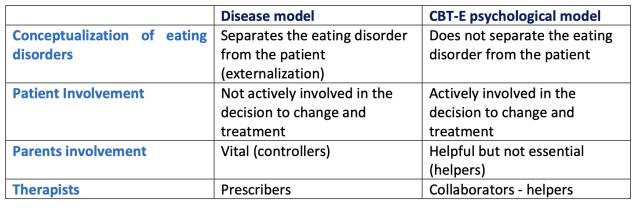
Contrary to the disease model, the psychological model adopted in CBT-E never requires patients to do anything against their will. During the two assessment/preparation sessions, patients are asked to consider the pros and cons of starting Step One—not necessarily to change—providing them with an opportunity to better understand the psychological function and maintenance mechanisms of their eating disorder. This helps them to be in a better position to evaluate the implications of changes.
Moreover, the goal of Step One in CBT-E for underweight patients is not weight restoration but rather understanding the psychological nature of their eating disorder and actively deciding whether to address changes, including weight recovery. In other words, the objective of CBT-E is for the patient to decide to recover weight rather than having this decision imposed by the therapist. This strategy is also applied to other ego-syntonic characteristics of eating disorder psychopathology, such as dietary restriction and restraint and excessive exercise.
A key strategy in CBT-E is to collaboratively create a personalized formulation of the main processes maintaining the patient's eating problem, which becomes the treatment target. The patient is educated about these processes and actively involved in deciding to address them. If the patient does not conclude that there is a problem to address, treatment cannot begin or must be postponed, although this is a rare occurrence.
The patient is instructed to observe how the maintenance processes of their eating problem operate in daily life. They are asked to monitor their eating in real time and the events, thoughts, and emotions influencing it. Subsequently, the patient is encouraged to make gradual behavioral changes within the context of their formulation and analyze the effects and implications on their thinking. In the later stages of treatment, when the main maintenance processes of the eating disorder have been interrupted and the patient reports periods free from concerns about weight, body shape, and eating control, the treatment helps them recognize early signs of the eating disorder mindset and quickly detach from it, thus avoiding relapse.
Parents, also with the help of specific educational videos, are actively involved in creating an optimal family environment to facilitate the adolescent's change and, with the adolescent's agreement, support them in implementing some CBT-E procedures.
Effectiveness of CBT-E for Adolescents
Several studies have evaluated CBT-E's effectiveness for adolescents aged 11 to 19. Seventy-two percent of patients with anorexia nervosa completed outpatient CBT-E, with 62 percent achieving complete remission at follow-up. A non-randomized efficacy study at Children's Hospital of Minneapolis found CBT-E's outcomes similar to FBT at 6 and 12 months post-therapy.
The CogFam Norwegian Trial
In 2024, the CogFam trial, a non-inferiority randomized control study, commenced patient recruitment to evaluate the efficacy of CBT-E versus FBT for adolescents aged 12 to 18 with eating disorders. The study spans eight outpatient clinics across four regions in Norway: Oslo, Bergen, Trondheim, and Tromsø.
By comparing these treatments, the CogFam trial hopes to shed light on which approach might be more effective for specific subgroups of patients, thereby enhancing treatment personalization in the management of eating disorders.
Conclusions
CBT-E is a promising treatment for adolescents with eating disorders and offers several clinical advantages. It is well-accepted by both young people and their parents. The collaborative nature of CBT-E is particularly beneficial for ambivalent young patients who may be especially concerned about issues of control. Additionally, it accommodates parents who may not be able to participate in all treatment sessions.
References
Dalle Grave, R., & Calugi, S. (2020). Cognitive Behavior Therapy for Adolescents with Eating Disorders. New York: Guilford Press
Dalle Grave, R., & el Khazen, C. (2022). Cognitive Behaviour Therapy for Eating Disorders in Young People: A Parent’s Guide. London: Routledge.
Dalle Grave, R., & Calugi, S. (2024). A Young Person’s Guide to Cognitive Behaviour Therapy for Eating Disorders. London: Routledge.




