Memory and Mental Health
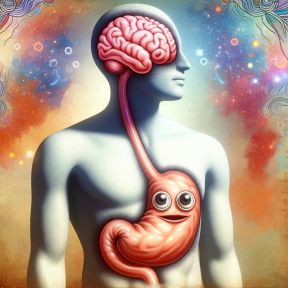
Memories can be immensely powerful, and for people struggling with mental health conditions, that power can be a burden. Memory keeps a record of what has made someone uneasy or upset, what undercut a person’s sense of self-worth, what brought extraordinary shock or pain. Also, perhaps, the unhealthy habits that have provided temporary relief. Because memory has an important role in pathological thinking and behavior, however, what scientists and clinicians have learned about memory can also be key to helping people recover from mental illness.
On This Page
Widespread mental health conditions such as depression, substance use disorders, and anxiety disorders have complex causes that differ substantially. Yet it is clear that each is characterized, in some ways, by how memory works in the people who suffer from them. And the experience of psychological stress—something known to every human, but which surfaces intensely in a range of disorders—is well established as a force affecting how we remember.
Stressful situations (such as when someone narrowly avoids a threat) can result in strong future memories about the experience. But during a stressful event, remembering information can be more challenging than usual. Over time, chronic stress and elevated levels of stress hormones like cortisol may have a detrimental effect on the ability to remember. Taking steps to reduce stress is one way people can seek to preserve memory ability.
Depression is associated with multiple kinds of cognitive impairment, including forgetfulness— though memory difficulties often resolve after a depressive episode is successfully treated, according to the DSM-5. A depressed person may also show other memory differences, including relatively weak memory for positive events, stronger memory for negative ones, and relatively general (rather than specific) recollections about personal experience. Depression has been linked with reduced volume in the hippocampus, a part of the brain that is important for memory.
Differences in how depressed individuals frame their experiences, past and present, may worsen other symptoms of depression. If someone who has depression is biased to recall negative memories, the increased rumination about negative experiences may in turn contribute to depressed mood.
Memory plays a central role in addiction: The formation of an addictive habit and the cravings that perpetuate it rely on connections in memory between particular situations, behaviors, and feelings that typically surround them, including the anticipated high of drug use, for instance. These associations remain in memory after drug use ceases, and so exposure to cues linked drug use can pose a risk of relapse.
Intoxication from a range of addictive substances, including alcohol, opioids, and sedative, hypnotic, or anxiolytic drugs can impair memory in the short term. Blackouts are a form of temporary amnesia caused by heavy drinking. In the long term, severe substance misuse, including alcoholism, can lead to more lasting impairment in memory ability. In some cases, chronic alcohol misuse leads to Wernicke-Korsakoff syndrome, which involves potential severe memory loss and inability to form new memories.
Anxiety disorders rely on associations formed in memory, including those between a stimulus—whether it is a social situation, an intrusive thought, a certain kind of animal, or something else—and the reflexive responses someone typically has to it. Accordingly, some forms of treatment for conditions such as generalized anxiety disorder or social anxiety disorder aim to change the nature of these learned associations. Exposure therapy is, in essence, a learning experience: By allowing people with anxiety to encounter threatening stimuli in a psychologically safe way, it is designed to create new memories and by doing so, alleviate the anxious response.
High levels of anxiety may have a detrimental impact on certain kinds of memory, particularly working memory, research suggests. This may be partly due to increased difficulty with disengaging from threatening distractions. However, the evidence on whether people with high anxiety have worse long-term memory is mixed.
Memory extends the reach of traumatic experiences—shocks to the system such as acts of violence or abuse or a life-threatening accident—allowing them, in many cases, to continue to disrupt the lives of those who had them long after they occur. Post-traumatic stress disorder is marked, in part, by upsetting and uncontrolled memories, which trauma-focused therapies are used to help defuse.
After someone suffers a traumatic experience, common reactions include mentally replaying the memory of the experience. Recurring, involuntary, and intrusive distressing memories are one symptom of post-traumatic stress disorder. Sometimes, when the memory of a trauma is cued by an experience in the present, the individual may feel as though the traumatic experience is happening again—a reaction commonly called a flashback. Given that these forms of re-experiencing can be highly distressing, it is also common for someone who has lived through trauma to try to avoid thinking about the experience and to avoid cues that may trigger the memory of the experience.
A variety of things can remind someone of a traumatic experience and potentially cause distress or other forms of re-experiencing. These cues may include places, people, or other things related to the traumatic event(s), such as a location close to where the event occurred, a person who looks like the one who caused the trauma, or a situation that resembles, in some way, that in which the traumatic experience occurred. They may also include internal physiological states associated with the experience.
There are a range of therapeutic approaches to recovering from trauma, which involve, in part, processing traumatic memories and reducing their negative impact. Among these are evidence-supported types of therapy such as prolonged exposure (PE) therapy, cognitive behavioral therapy (CBT), and eye movement desensitization and reprocessing therapy (EMDR). Effective treatment helps individuals who have experienced trauma safely face the experience and can decrease the power of traumatic memories.
Yes. Some parts of the experience, including those a person who experienced the trauma was most focused on in the moment and the emotional impact of the trauma, are often preserved clearly in long-term memory. But more peripheral information, such as details about the situation that are not personally salient at the time, or about the broader period of time in which an event happened, may not be remembered—and incomplete memories of trauma can still be reliable. In some cases, even central details may not be saved in memory due to the impact of intense stress. Aspects of a traumatic experience that are initially remembered may also be forgotten over time, or not thought of for a period of time and remembered later.
After a traumatic experience, a person may try to avoid memories of it, a behavior sometimes called suppression. In therapy, someone who has avoided details of a traumatic memory may be encouraged to recall them in a careful, guided way as part of treatment. However, the idea that the memory of a traumatic experience can be automatically, unconsciously repressed because of the impact of the trauma—made inaccessible to the person who had the experience, but recoverable through special therapeutic interventions—is more controversial and has been challenged by scientists who study memory.
Scientists have investigated the possibility of using certain drugs, including the beta-blocker propranolol, to treat post-traumatic stress disorder. In such interventions, the drug is administered to individuals either shortly after they have experienced a traumatic episode—with the aim of blocking initial memory consolidation—or prior to reactivating memories of the trauma, which is thought to influence the reconsolidation of the memories. Some researchers have reported significant reductions in symptoms of PTSD following these treatments, though there is a need for further research on their effectiveness.