Suicide
Real-Life Suicide Assessments: Who, What, When, How
Don't make the same mistakes Hollywood does in portraying suicidality
Posted January 12, 2013
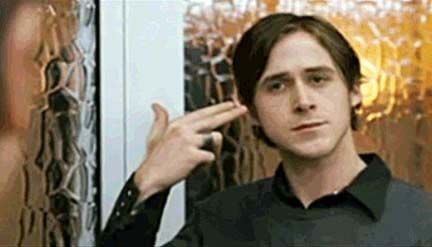
Gosling's character informs McGregor's that he's going to kill himself.
In the 2005 film Stay, a suicidal client played by Ryan Gosling informs Ewan McGregor’s psychiatrist character, Sam, that he intends to kill himself in 3 days.
McGregor’s character proceeds to freak out (which doesn’t make sense; most therapists deal with suicidality on a regular basis), lunging for the phone (which could violate confidentiality, since a therapist needs to be sure there’s truly a life-or-death emergency before telling anyone) and then, after Gosling leaves, seeking out a friend who works in a hospital psych ward to “check the protocol on involuntary committal.” (Any therapist who doesn’t know the protocol on involuntary commitment needs to stop practicing and get some supervision immediately!)
The movie then portrays the hospital as a horrifying place where the doctors are jaded and screaming patients are regularly tackled and forcibly injected with medications. Even the doctor McGregor consults says it’s a horrible place for patients to be. (Frankly, most hospitals aren't that bad of a place to be if you need the help. But portrayals like this certainly keep people from wanting to go if they need to!)
(Note: "The 'twist' of the film makes all of the characters' behaviors work, even the inaccuracies, but in real life many of Sam's and Henry's behaviors would be seen as inappropriate, and the way psychology is practiced in the movie is not adhering to ethical or sometimes even practical standards.)
What is a Suicide Assessment?
Suicide assessments are informal evaluation processes psychological professionals go through to decide
- Whether a client might be suicidal and
- How immediate any danger is
When is a Suicide Assessment Done?
Typically as part of the initial intake interview, and any other time that a client indicates possible suicidal ideation (thoughts about suicide) through speech or behavior.
Who Does the Assessment?
Sometimes the client is in the office when he indicates that he has suicidal ideation, but sometimes a concerned friend, family member, or even coworker will call. If the therapist already sees the person in question, it's her job to assess the client's present state of mind. If the person in question isn't the therapist's client, she'll advise the caller to go to the nearest emergency room or crisis center.
Immediate Danger
If the client is clearly in immediate danger of harming himself, the therapist will ask the client or caller to go directly to the closest hospital's emergency room. All emergency rooms have a social worker available to decide whether the person should be admitted.
If the client is going to be admitted, the therapist will often meet her at the emergency room. Thanks to the red tape of insurance, it's not uncommon for the admittance process to take 3 to 5 hours, which means a lot of sitting around the waiting room.
Less Immediate Danger
If the caller or client isn't in immediate danger but is still feeling unsafe, the therapist will ask him to come in for an emergency appointment. She'll probably encourage him to have someone drive him, not only because it's safer for him (and probably the other folks on the road), but also so the client has a ride and emotional support if he does need to go to the hospital.
How is the Suicide Assessment Done?
A therapist never talks to anyone outside the office about a client unless she has the client's written permission (for example, because she's consulting with another of the client's doctors) or the client is in immediate danger. That means that when suicidality is involved, she must assess whether the situation is serious enough to involve other people. Every suicide assessment contains three parts: plan, means, and time. The therapist asks:
- If the person knows how he would harm himself (plan).
- If he has the means to do it (means).
- If he has a time planned (time). People who are serious often do, or they may just say, "I can't stand it anymore," which pretty much means "now." If someone doesn't have a clear and immediate answer to this question, the therapist may ask, "Can you be safe?" or "Can you stay safe if you go home?" Someone who is really in trouble will generally say, "No."
Therapists can usually tell pretty quickly how urgent the situation is, mostly because people have little problem telling them! Obviously, if someone is in so much emotional pain that he'd rather die than finish the day, the hospital is the next stop.
Involuntary Hospitalizations
Psychiatric hospitalization is like any other hospitalization. The doctors work hard to provide symptom relief as fast as possible, and keep the person in an environment where if there's an emergency, someone is there right away to help. And the hospital may be the only place the problem can be properly treated—the bone will be set, the person with pneumonia is given antibiotics to help the body's natural immune systems fight off infection, and the person who's suicidal will usually be given medication and therapy that will quickly help stabilize brain chemicals.
Involuntary hospitalizations are actually rarer than the average person thinks: most people who feel this bad really just want to feel better, and if that means going to the hospital, they're ready to go! You also have to remember that people who really want to die don't typically tell anyone. They just do it. If someone realizes your character is suicidal, it's because he's struggling to keep himself going. People who do commit suicide do so because they've reached the point where they see no other solution.
In the rare situation that a client really doesn't want to go to the hospital and is really in danger of killing himself, the therapist can explain that she's legally and ethically obligated to do everything she can to keep him safe, up to and including involuntary hospitalization. Then she explains (and this works better if the therapist can say this kindly) that the police are the ones responsible for taking him to the hospital, which means he's likely to end up in the back of a squad car. In the end, most people agree that it's a lot easier to just go voluntarily.
Safety Plans
If the client believes he can stay safe for a given period of time (say, a week—asking a client to stay safe for one week at a time is reasonable) and can promise to tell someone or go to the hospital if that changes, he and the therapist may create a Safety Plan. In a safety plan, the client promises (often in writing) that he will not harm himself, and if he feels he can't hold to that, he has a series of things to do, in the order he should do them. Usually safety plans include things like calling a trusted friend, asking someone to come over and stay, calling the therapist, and going to the emergency room.
Though all of these steps are taken for both clinical and legal purposes, having done all of these things correctly doesn’t necessarily protect the therapist from a lawsuit if the individual kills himself.
Using the Information in Your Story
Though it can feel stilted to include the assessment in your story if you're not quite sure how one would go in real life, the assessment is usually where the most important (and interesting) information is revealed. Knowing that your character not only plans to shoot himself but also has a gun in the car and intends to drive out to a field after the session and do it, for example, forces the therapist to take immediate action.
Men are more likely to use violent means like guns, while women are more likely to do things they can "change their minds" on, like taking pills or slitting their wrists. Women attempt suicide more often, but men complete suicide more often.
The Aftermath of Suicide and Suicide Attempts
Some people time their attempt so someone can "accidentally" find them, and people who change their minds often call 911 or ask someone else in the building for help. Those who slit their wrists usually have "hesitation" or "practice" marks, which are shallower cuts they make while they're working their way up to something that's actually deadly. Many people who actually die during a suicide attempt probably didn't mean to.
Also think beyond the drama of an actual suicide. One of the most horrible things anyone can face is finding the body of someone who killed himself, because there are always self-recriminations. People who commit suicide have often thought about how it will affect those left behind: they have been known to lay out plastic to make sure blood is easy to clean up, to kill themselves away from home (like in a hotel room), or to use methods they believe will be "cleaner" than others, like closing themselves in a garage with a car engine running. (Note: there is no clean method—carbon monoxide poisoning suffocates every cell in the body, and that doesn't make for a pretty corpse).
People also screw up suicide attempts, making their problems worse. A bullet to the head isn't always deadly, and people have taken full shotgun blasts in the face and survived. In 2005, a man who intended to kill himself by driving his SUV onto commuter train tracks panicked at the last minute and ran from the SUV; unfortunately, the people on the train didn't have that option, and 11 were killed and nearly 200 were injured. Juan Manuel Álvarez was subsequently arrested and found guilty of 11 counts of first degree murder and one count of arson; in 2008 he was sentenced to 11 consecutive life sentences.
For more information on using accurate psychology in your writing, check out The Writer's Guide to Psychology: How to Write Accurately About Psychological Disorders, Clinical Treatment and Human Behavior. More information is available on the book's website.
© 2013 Carolyn Kaufman, PsyD ♦ Psychology for Writers on Psychology Today




