Fear
COVID-19 Fear and the Behavioral Immune System
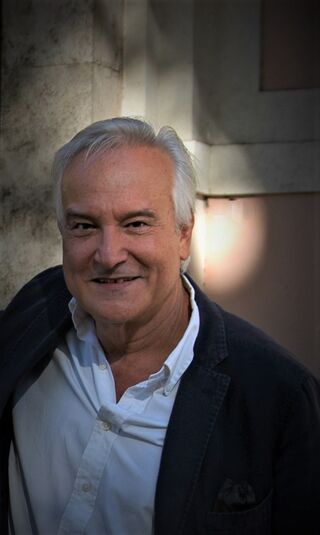
An interview with Dr. Alfonso Troisi on the origins of pandemic fear.
Posted July 22, 2020
The coronavirus pandemic has caused many to live in fear and anxiety, especially of catching the disease itself. These fears can further turn into xenophobia or even panic. The following interview with Dr. Alfonso Troisi explores an evolutionary perspective on this COVID-19 fear.
Alfonso Troisi is Professor of Psychiatry at the International Medical School of the University of Rome Tor Vergata. In addition to 250 research papers and book chapters, he has published three books: Darwinian Psychiatry (1998, Oxford University Press), The Painted Mind: Behavioral Science Reflected in Great Paintings (2017, Oxford University Press), and Bariatric Psychology and Psychiatry (2020, Springer). The common theme of his research and clinical activity is the application of evolutionary science to the study of human behavior and mental disorders.
JA: How did you first get interested in this topic?
AT: The COVID-19 pandemic has so many implications for public health and social organizations that disparate scientific disciplines from virology to economic science have been asked to contribute intervention strategies and preventive programs. I am a clinical psychiatrist with a long-standing interest in the application of evolutionary science to medical problems. Discussing with my colleagues, interviewing patients, and navigating social media, I realized that the COVID-19 pandemic is perceived and analyzed from a variety of perspectives except from an evolutionary point of view. This is a paradox, considering that infectious disease has been a major challenge during our evolutionary history. We cannot get a full understanding of the psychological and social consequences of the COVID-19 pandemic if we ignore how the risk of infectious disease shaped the evolution of the human mind and behavior.
JA: What was the focus of your study?
AT: The focus of the study was on the psychological and social consequences of the COVID-19 pandemic as explained by the activation of the behavioral immune system. As most may know, the physiological immune system is our body’s defense against infections. Yet, this is not the only defense we have. Natural selection has favored the parallel evolution of a behavioral immune system that is separate from, and complementary to, the physiological immune system. Like the physiological immune system, the behavioral immune system includes both detection and response mechanisms. When an external cue connoting infection risk (e.g. seeing another person with evident manifestations of infectious disease) is detected, it triggers a cascade of emotional, cognitive, and behavioral responses that minimize the infection risk (e.g. through social avoidance of people who appear to pose an infection risk). The study analyzes the emotional responses to the risk of catching the new coronavirus from an evolutionary perspective.
JA: What did you discover in your study?
AT: Evolutionary predictions on people’s emotional reactions to infection risk have been confirmed by observations of individual and social behaviors during the COVID-19 pandemic. When the threat of pathogen infection is salient, people are likely to be hypersensitive to inferential cues that discriminate between familiar and foreign persons. The social ecology of ancestral humans explains the link between the behavioral immune system and xenophobia. For most of their evolutionary history, humans lived in widely dispersed, nomadic, small populations made up of individuals with a high degree of familiarity. Such a kind of social ecology minimized the risk of getting infectious diseases. By contrast, contact with foreign people who were hosts of exotic pathogens could be especially virulent for a local population.
Obviously, the identification of any foreign person as a potential source of contagion is often an erroneous over-generalization but, from an evolutionary perspective might say, “better safe than sorry.” Xenophobia elicited by fear of infection is well-illustrated by the alarming tendency to associate the new coronavirus with foreign nationals and foreign countries. For example, President Donald Trump has called the coronavirus the “Chinese virus” or the “Kung Flu” and Thailand’s public health minister said that white foreigners were dirty and spreading the virus in the country, adding that people should be more afraid of Westerners than Asians.
JA: Is there anything that surprised you in your findings, or that you weren't fully expecting?
AT: I was surprised by the stressful impact of social distancing on people’s psychological well-being. We belong to a social species of primates with a strong need for physical contact. The new technologies (e.g. video chat software, social media groups) helped reduce the stress of the lockdown but they are not “the real thing.” As a clinical psychiatrist, I saw people reporting depressive and anxiety symptoms caused by the lack of physical contact with relatives and friends, even if other forms of social interactions were still possible.
JA: How might readers apply what you found to their lives during COVID-19?
AT: The psychological responses activated by the behavioral immune system evolved to afford adaptive benefits in a socio-ecological environment that was substantially different from modern environments. In small bands made up of individuals with a high degree of familiarity, fear of immigrants, and social conformity were effective means to reduce the risk of contagion. In the “global village” where we live, xenophobia, intolerance of dissent, and preference for authoritarianism are useless reactions that can negatively impact social organization. The take-home message of the study is that our emotional reactions to the pandemic are largely driven by primitive adaptations. The antidote against irrational fear consists of rejecting fake news and trusting scientific data.
JA: How can readers use what you found to help others amidst this pandemic?
AT: Mental health professionals helping people stressed by the COVID-19 pandemic should acknowledge that there is a substantial difference between fear of infection and fear of serious diseases that are common in ordinary times (e.g. fear of cancer, Alzheimer’s disease, and heart disease). Fear of non-infectious diseases is largely cognitive and prompted by cultural inputs. By contrast, fear of infection is deeply rooted in our emotional brain. Treating fear of infection as an emotional response worthy of professional intervention may trigger the undesirable effects of pathologizing a normal condition. For example, the decision to implement crisis interventions for a small group of healthcare workers who are facing the COVID-19 pandemic should be carefully evaluated in the light of findings that show an increase in post-traumatic stress disorder (PTSD) symptoms after trauma debriefing compared with control treatments.
JA: What are you currently working on that you might like to share about?
AT: I am currently conducting a study on individual differences in emotional reactions to the COVID-19 pandemic. Some people are extremely scared by the risk of catching COVID-19. Others seem to underestimate the risk and are intolerant of the restrictions imposed by public health authorities. My aim is to discover which individual variables (e.g. age and gender) and personality factors (e.g. impulsivity and attachment style) can explain different levels of fear of infection. Perception of risk and propensity to engage in risky behaviors depend in part on psychological mechanisms that are related to our evolutionary heritage. I want to investigate the role of these mechanisms in modulating individual emotional reactions to the COVID-19 pandemic.
References
Troisi, A. (2020). Fear of COVID-19: Insights from evolutionary behavioral science. Clinical Neuropsychiatry: Journal of Treatment Evaluation, 17(2), 72–75.


