Eating Disorders
Addressing Cessation of Binge Eating and Weight Loss
A new integrated and personalized treatment for binge-eating disorder.
Posted May 26, 2020
Binge-eating disorder (BED) is the most common of the specific eating disorders, occurring across ethnic and racial groups, among both men and women and in adults of all ages. It is accompanied by high levels of distress, psychiatric morbidity, and psychosocial impairment. The majority of patients who seek treatment for BED are also overweight or obese, although the diagnostic criteria do not require that that be the case.
The best available psychological treatments for BED, such as cognitive behavior therapy (CBT), interpersonal psychotherapy (IPT), guided self-help based on CBT (CBTgsh), produce good and lasting outcomes with regard to control over eating but virtually no weight loss. However, both control over eating and weight loss are important and valued goals of those who seek treatment.
Traditional behavioral weight-loss intervention (BWL) produces a reduction in binge eating as well as modest weight loss. Unfortunately, the effects of BWL in terms of the cessation of binge eating are not as well maintained as in CBT and the weight lost is generally regained.
The data on the treatment outcome of BED indicate there is need for a new therapeutic approach that produces clinically significant, albeit modest, weight loss as well as the remission of binge eating. Available data indicate that patients abstinent from binge eating maintain their end-of-treatment weight, including any modest weight loss that may have been achieved during treatment.
Zafra Cooper, from the University of Yale, my colleague Simona Calugi and I have developed a new treatment for BED designed to overcome the limits of existing approaches. The treatment aims to achieve both the cessation of binge eating and weight loss.
The first step was to develop a model of the key maintaining factors maintaining both the binge eating and the overweight/obesity. (see Figure 1). Using this model, treatment can be individualized to target the most salient processes for each patient, thus making it particularly suitable for a variety of different clinical presentations that characterize patients with BED.
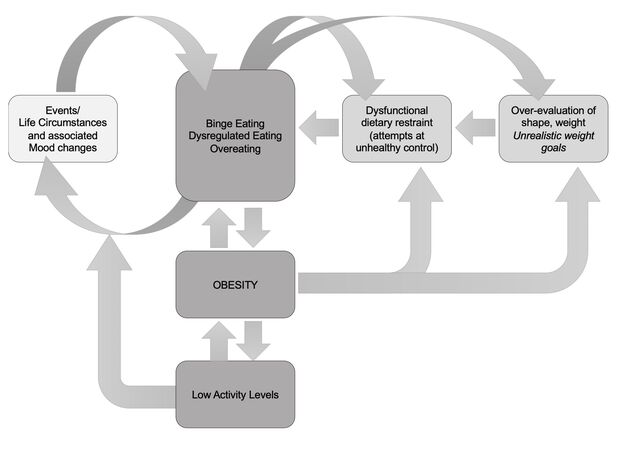
The model integrates mechanisms maintaining binge eating from the transdiagnostic theory of eating disorders (light grey shading) that forms the basis for empirically supported enhanced cognitive behavior treatment (CBT-E) with those factors that maintain obesity (shown in dark grey shading). It is suggested that, as with other eating disorders, over-evaluation of shape and weight, extreme and inflexible forms of restraint (when present), and the effects of events and moods (light grey shading) maintain BED although not all maintaining factors apply in all patients. The model includes also additional maintaining mechanisms that often operate in overweight/obesity such as dysregulated overeating unstructured eating, unhelpful food choices, etc), high levels of inactivity, and unrealistic weight expectations and related life goals.
The second step was to design a new treatment based on the model described above that has the goals of controlling binge eating and achieving modest weight loss through a sustainable and flexible form of dietary restriction. The proposed integrated treatment is modular and thus may be personalized to focus on individual maintaining mechanisms that operate in any individual case rather than being based on a uniform “one size fits all” model. It incorporates elements from two previously tested evidence-based interventions, CBT-E for eating disorders, shown to be effective in reducing binge eating and CBT for obesity producing, at least in the short term, weight losses of 6.8% of initial body weight at the end of treatment with 71% of patients achieving a weight loss of ≥ 5% as well as significant improvements in eating disorder psychopathology.
After an initial assessment appointment, the active treatment consists of 24 sessions over 24 weeks followed by an extended maintenance phase with at least monthly short check-in sessions over the year following the end of treatment (see Figure 2).
The proposed treatment has four distinct phases. The first two stages are relatively uniform for all patients, although even at this stage the start of formal weight loss procedures is individualized depending on initial progress, with formal weight loss being introduced earlier for those whose binge eating reduces rapidly. While the main body of treatment (stage three) will always include a weight loss component, its content will be individualized to include modules relevant to the patient’s personal formulation and its re-assessment in stage two. Stage four focuses on maintaining changes made in treatment to maintain progress in the long term. To achieve maximum early change, consistently associated with a better outcome, it is proposed that the first stage of treatment should involve twice-weekly sessions for 4 weeks, followed by weekly sessions for the main body of treatment and sessions every 2 weeks during the last stage of treatment that focuses on maintaining changes in the long term.
The subsequent maintenance phase would be over 12 months and involve monthly short appointments, preferably completed remotely via telephone or videoconferencing.

An essential next step is to assess whether the new proposed treatment outperforms the current best available treatments for those with BED and accompanying overweight and obesity. This would require it to achieve similar outcomes with regard to the control of binge eating as those achieved by current best practices while also achieving moderate and clinically significant weight loss that is maintained over time. Should these two outcomes be achieved, there would also be indirect support for the proposed model.
This post was co-authored by me and Zafra Cooper, DPhil, Department of Psychiatry, Yale Medical School, Yale University, New Haven, CT, USA
References
Cooper Z., Calugi S., Dalle Grave R., “Controlling binge eating and weight: a treatment for binge eating disorder worth researching?”, Eating and Weight Disorders 2019 Jun 18. doi: 10.1007/s40519-019-00734-4


