Coronavirus Disease 2019
Does COVID-19 Target the Brain?
New study shows increased rates of psychiatric illness after COVID-19.
Posted December 7, 2020 Reviewed by Lybi Ma
As the worldwide pandemic grips every corner of the globe, the severe stress on humans is causing higher than usual rates of mental health symptoms across populations. A recent study, "Impact of COVID-19 pandemic on mental health in the general population: A systematic review," shows increases in anxiety, depression, post-traumatic stress disorder (PTSD), and other emotional difficulties increasing in all populations during this period of instability, loss, and loneliness.
Beyond these challenges, researchers also have wanted to know whether this new type of coronavirus has specific effects on mental health. In a recent study “Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62,354 COVID-19 cases in the USA,” researchers explored whether getting sick with COVID-19, independent of other stressors, could affect the brain in ways that cause psychiatric or neuropsychiatric symptoms.
We already know that the virus that causes COVID-19 (SARS-CoV2) and the body’s immune response to this virus affect many organs and tissues beyond the lungs and respiratory system. Having COVID-19 can damage blood clotting systems, kidney function, and heart muscle, for example. COVID-19 also affects nerve cells, leading people to lose their sense of smell. And many people who are infected with SARS-CoV2 experience “brain fog,” which means it has some effects on brain cells. The question here is whether a diagnosis of COVID-19 has effects on the brain that could lead to psychiatric diagnoses?
This study tried to answer this question by reviewing the medical records of over 60,000 patients who had been diagnosed with COVID-19 and comparing them to matched groups of people who were diagnosed with other health problems at the same time. When researchers looked at their results, the data suggested that a COVID-19 diagnosis increased the likelihood of a psychiatric diagnosis, and it increases this risk more than having another illness would. Their results support the possibility that something particular about this novel coronavirus infection may be triggering mental health events.
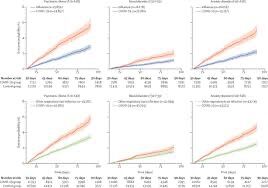
The comparison groups included people diagnosed with the flu, other respiratory illnesses, skin infections, gallstones, kidney stones, or a fracture in one of the large bones of the body. The people with those diagnoses had some increased risk of psychiatric diagnoses in the 14 to 90 days after becoming ill (or suffering a fracture). But the group with COVID-19 had even higher risks, about twice the risk, of getting a first diagnosis of any psychiatric disorder in the same time frame. This comparison points to an increased risk of a psychiatric illness related specifically to COVID-19.
The psychiatric conditions having the highest risks associated with COVID-19 were anxiety disorders, including generalized anxiety, adjustment disorder, panic disorder, and PTSD. Next most likely were mood disorders, most often depression. Insomnia (with or without anxiety) and dementia diagnoses, especially in those over 65, were also statistically more common following COVID-19 than following other illnesses or a fracture.
The data showed that patients with more severe COVID-19, people who had to be hospitalized, had the highest rates of psychiatric illness. The researchers wondered if just being so sick, rather than being sick specifically with COVID-19, was the primary reason for the increased psychiatric symptoms. However, even when they took out the sickest people in all of the groups (COVID-19 and the other illnesses) and just looked at people who didn’t need hospitalization, the COVID-19 group had higher rates of psychiatric illness than those who experienced other medical conditions.
The researchers also looked at the time frame or context of the conditions, thinking that maybe anyone who was sick with anything during the pandemic period (after April 2020) might have a higher likelihood of anxiety, depression, or insomnia. This was not the case, even within this time frame, people with COVID-19 were more likely than those with other illnesses to suffer from anxiety and other mental health problems.
This research is preliminary, and we need much more data to parse these possible connections, but it would not be surprising if this virus was found to affect parts of the brain that lead to psychiatric illness. The virus and the immune responses it triggers can cause tremendous damage to a variety of organs in the body. The brain is a sensitive organ and could well be affected by the virus itself or by the powerful cascade of responses that the body generates to try to fight off COVID-19. These are possible explanations but need much more detailed study to understand clearly.
Even though we need many more studies in this area, the results from this review strongly indicate that we need to pay attention to mental health evaluation and treatment for people who have been diagnosed with COVID-19. While everyone in the world is being impacted by the pandemic, and risks are higher for depression and anxiety symptoms all around, those who are infected with the virus may be at a heightened risk for psychiatric problems, and we must not forget that part of their overall health and recovery.
References
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., … McIntyre, R. S. (2020, December 1). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders. Elsevier B.V. https://doi.org/10.1016/j.jad.2020.08.001
Maxime Taquet, Sierra Luciano, John R. Geddes, and Paul J Harrison. November 9, 2020. “Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA” in The Lancet https://doi.org/10.1016/S2215-0366(20)30462-4.




