Sleep
Taking Melatonin but Still Can't Sleep?
Melatonin plays an important role in sleep, but it may not be the one you think.
Updated May 23, 2024 Reviewed by Gary Drevitch
If you're among the millions of Americans desperate for a good night's sleep, you may have tried an over-the-counter sleep aid. Sch medications may contain diphenhydramine (e.g., Unisom, Zzzquil, Tylenol/Advil PM), an antihistamine also found in allergy medications like Benadryl. Diphenhydramine is a sedative, which many of us have realized only after taking it for allergies and then feeling knocked out at work.
Another common OTC medication often taken for insomnia is melatonin. About half of the people who come to me for insomnia treatment are taking melatonin, which suggests that, at least for these individuals, it's not a very effective treatment. In fact, the most recent meta-analysis of studies found that melatonin supplements provide about 8 minutes of additional sleep per night compared to a placebo. If you're starved for sleep, anything beats nothing, but for many people 8 minutes will be just a drop in the bucket. To understand why the effect is so small, let's consider what melatonin is and how it's related to sleep.
What Is Melatonin?
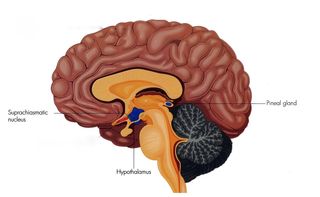
Your body produces the hormone melatonin in the pineal gland, a small structure that sits just above the brainstem at the midline of the brain (see figure at left). The pineal gland is controlled by a center within the hypothalamus—the suprachiasmatic nucleus—that regulates our circadian rhythm.
Thanks to this roughly 24-hour cycle, major bodily functions like sleeping, waking, body temperature, hormones, and metabolism are aligned with the cycles of light and dark, as well as with all the activities that coincide with day and night. If you've ever been jet-lagged, you know how disruptive it is to have your internal cycle and external demands misaligned.
The timing of melatonin release is consistent with its relation to sleep. Very little is released during the day, with levels rising as the sun goes down and bedtime approaches. Melatonin levels peak in the middle of the night, and fall to their daytime lows as we approach our wakeup time and the sky begins to lighten.
Given the increase in melatonin as sleep approaches, it's reasonable to expect that taking extra melatonin would facilitate sleep, especially at the high doses of 3, 5, or even 10 mg often sold in drug stories. (Several research studies of melatonin used doses of just .1 or .3 mg). So why only 8 minutes of additional sleep?
The Role of Melatonin in Sleep
In humans, who generally sleep at night, melatonin levels rise after sunset. In rodents and other vertebrates that are active at night, melatonin levels also rise at night. That's right: The same hormone is linked to opposite patterns of behavior, depending on the species.

For example, when researchers continuously measured melatonin levels in mice, they found a strong connection between higher melatonin levels and greater activity. (For a review on the physiological effects of melatonin, see this article.)
So what melatonin actually seems to be doing is sending a signal for "typical nighttime behavior." If you're a human or other "diurnal" (active during the day) species, that signal will mean "go to sleep." For a mouse, that same signal means to sneak into your kitchen and forage for food. And if you battle chronic insomnia, your typical nighttime behavior might be staring at the ceiling and praying for sleep.
No wonder melatonin doesn't tend to be a great sedative. It's not like an antihistamine or a benzodiazepine that have inherently tranquilizing effects; that's not its function. Instead the role of melatonin is to match our internal clocks with external demands, particularly those aligned with light-dark schedules.
Recommended Treatments
In light of the limited evidence for melatonin's effectiveness as a sleep aid, current clinical guidelines recommend against its use in the treatment of chronic insomnia. These guidelines list other types of medication (e.g., zolpidem, eszopiclone; trade names Ambien, Lunesta) that may be better options based on their demonstrated efficacy.
The guidelines also recommend that any medication be paired with a treatment like cognitive behavioral therapy for insomnia (CBT-I). While some medications can be as effective as CBT-I in the short term, CBT-I has a better track record for helping in the long term, even without medication. (You can read about the basics of CBT-I here.)
Unfortunately, the best therapies are often the hardest to find. If there is no CBT-I expert close to you or in your insurance network, there are other options available so you can still have the benefit of this treatment. One option is to use a CBT-I app. One benefit of an app is that it can make it easier to record and analyze your sleep data, an essential part of the treatment. I can't personally vouch for any of these applications, but this review provides a helpful summary of some available options. There are also books that present CBT-I concepts; two that have received positive reviews are End the Insomnia Struggle and Quiet Your Mind and Get to Sleep.
So while melatonin won't cure most people's insomnia, there are other options that can be very effective, and, as in the case of CBT-I, they may involve no medications or side effects.
Melatonin for Shifting Sleep Schedule
While melatonin is not recommended for treating insomnia, the American Academy of Sleep Medicine does include it in its treatment guidelines for some of the sleep conditions related to circadian rhythm, consistent with its physiological function.
For example, many people experience "Advanced Sleep-Wake Phase Disorder," which simply means they're extreme night owls. In combination with other components like bright light at specific times, carefully scheduled melatonin can help shift one's circadian rhythm to better align with work and school schedules.

Care needs to be taken with the timing of melatonin supplements—too early or too late and it can just exacerbate the problem. Working with a specialist in behavioral sleep medicine generally is required.
If you've considered treatment for insomnia or another sleep disorder, now might be a good time to look into it. Better sleep helps with pretty much everything.
Disclaimer: As always, please check with your doctor before starting or stopping any medication.
References
Ferracioli-Oda E, Qawasmi A, Bloch MH (2013) Meta-Analysis: Melatonin for the Treatment of Primary Sleep Disorders. PLoS ONE 8(5): e63773. doi:10.1371/journal.pone.0063773
Nakahara, D., Nakamura, M., Iigo, M., & Okamura, H. (2003). Bimodal circadian secretion of melatonin from the pineal gland in a living CBA mouse. Proceedings of the National Academy of Sciences, 100, 9584-9589.
Pandi-Perumal, S. R., Trakht, I., Srinivasan, V., Spence, D. W., Maestroni, G. J., Zisapel, N., & Cardinali, D. P. (2008). Physiological effects of melatonin: Role of melatonin receptors and signal transduction pathways. Progress in Neurobiology, 85, 335-353.




