Autism
Opposite Genetic Profiles of Autism vs. Schizophrenia
Early onset of ASD compared to schizophrenia reflects oppositely in epigenetics.
Posted January 14, 2017
Although difficulties with social communication are symptomatic of both autism spectrum disorder (ASD) and schizophrenia, symptoms of ASD typically occur during early childhood, whereas most symptoms characteristic of schizophrenia do not appear before early adulthood. A new study has investigated whether the overlap in common genetic influences between these clinical conditions and impairments in social communication depends on the developmental stage of the assessed trait.
The study reports developmental profiles in common genetic overlap for both ASD and schizophrenia with respect to longitudinal measures of social communication difficulties within the general population. Analyses were based on the largest publicly available genome-wide data for ASD and schizophrenia, in addition to a large Danish ASD sample from the iPSYCH project and a well-studied UK birth cohort, the Avon Longitudinal Study of Parents and Children (ALSPAC).
Overlap in genetic influences between ASD and social communication difficulties during development decreased with age in the ASD samples, as might be expected of this early onset disorder. Genetic overlap between schizophrenia and social communication difficulties, by contrast, persisted across age as observed within two independent sub-samples, and showed an increase in magnitude for traits assessed during later adolescence—the typical age of onset. Both clinical ASD and schizophrenia were found to share some genetic influences with impairments in social communication but revealed distinct developmental profiles in their genetic links consistent with the onset of clinical symptoms, as illustrated below.
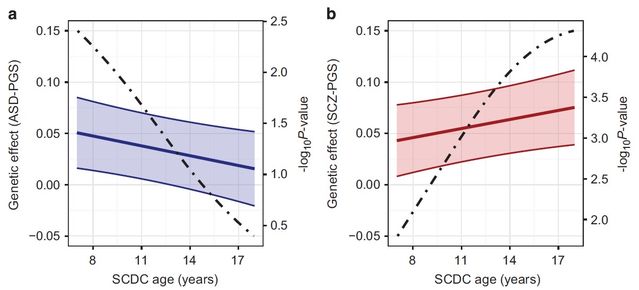
This study provided evidence for shared common genetic overlap between social communication difficulties and both ASD and schizophrenia, but does not imply a shared genetic susceptibility between these clinical conditions. Instead, we identified distinct patterns in genetic trait-disorder relationships, largely consistent with the onset of clinical symptoms. Genetic links were driven by independent polygenetic influences and showed opposite trends in magnitude with progressing age of the population-based trait, as supported by longitudinal analyses.
This is exactly what the diametric model predicts. According to this way of looking at it, ASD and schizophrenia are opposites: ASD is characterized by deficits in mentalism (aka people/social/communication skills) while schizophrenia exhibits hyper-mentalism epitomized in symptoms resulting from excessive mentalizing such as delusions of being watched, hearing voices, or being the subject of persecution. And just as both over-sensitivity and under-sensitivity to light or sound would result in visual or hearing deficits, so the diametric model proposes that both the hypo-mentalism of ASD and the hyper-mentalism of schizophrenia result in mentalizing difficulties. Nevertheless, the difficulties will be different, and their causes opposite, just as the authors' figure above and mine below illustrate.

Only the diametric model can explain why this is so, and can do so very readily. This is because it follows as a matter of necessity that, if ASD is characterized by symptomatic failure to develop normal mentalizing, such deficits will inevitably appear at the time mentalism is first developed: early childhood onwards. But because you have to acquire normal mentalistic abilities before you can take them to pathological extremes and because mentalism takes many years to master, the hyper-mentalism of psychoses such as schizophrenia normally only becomes apparent much later, typically during late adolescence or early adulthood. To this extent, schizophrenia and other such psychoses are comparable to other hypertrophic syndromes: giants have to reach normal size before they can become gigantic. Indeed, the model also explains why psychiatrists often report that some schizophrenics—strikingly unlike autistics—can show remarkable mind-reading abilities on occasions: hyper-mentalism isn't always misleading!
To this extent then, the new study vindicates, not only the diametric model of mental illness, but its core concept: a mentalistic continuum ranging from the hypo-mentalism of ASD to the hyper-mentalism of schizophrenia. And the fact that an opposite pattern of gene expression was found for each also of course corroborates the basic claim of the imprinted brain theory that genetic conflict is the fundamental factor. Indeed, a previous study of 1.7 million Danish health records which found birth size to be a reliable indicator of risk of mental illness as predicted by the theory underlines the parallel with hypertrophy in general, and more than hints that imprinted genes with their known links to growth are the specific agents in both ASD and schizophrenia.
(With thanks to Bernard Crespi for bringing this to my attention.)


