Autism
“Obese” Mothers and Autism: Not As Simple As It Seems
Mothers—no matter what their BMI—cannot be blamed for causing a child's autism.
Posted December 20, 2016
One of the many original and counter-intuitive predictions to which the imprinted brain theory gives rise is the suggestion that rising living standards may be a factor in explaining the so-called “autism epidemic” (first made by me in my book, The Imprinted Brain, in 2009, and repeated in a post on this site).
IGF2 is the paradigmatic imprinted gene, coding for a major growth factor, and is normally only expressed from the father’s copy. But in mice, a maternally active imprinted gene, Igf2r, contradicts its effects, mopping up the growth hormone, as explained in an earlier post. IGF2 has been found to be down-regulated in the offspring of women who have been starved during pregnancy, and so it would not be surprising if the same growth-promoting gene were up-regulated in the children of mothers who were fed better than normal. Indeed, a recent study using data from the Avon Longitudinal Study of Parents and Children cohort reported that "a prenatal maternal high-fat and -sugar diet may alter the DNA methylation status of the IGF2 gene at birth, which in turn, may increase risk for a range of psychiatric and health disorders." Furthermore, and as I noted in a previous post, a huge study of 1.7 million Danish health records established an unquestionable link between birth size and risk of mental illness: larger babies were more prone to ASD, but smaller ones to PSD, just as predicted by the imprinted brain theory.
Now a new meta-analytic study reports that
compared with children whose mothers were at normal weight, children born to overweight and obese mothers have a 28% and 36% higher risk of developing ASD, respectively. Maternal underweight was not associated with increased ASD risk. A linear dose-response relationship was found, with the risk of ASD increasing by 16% for each 5 kg/m2 increment in maternal BMI compared with that of normal weight.
Source: Wikimedia commons
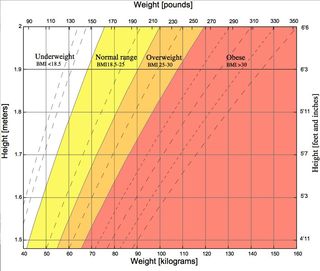
BMI stands for body mass index and is defined as your weight divided by your height squared, yielding the diagram left. The term was coined in 1972 by the nutrition and public health researcher, Ancel Keys, who explicitly stated that it was only appropriate for population studies and ought not to be used for individual diagnosis.
The problem to which the latter can give rise is illustrated by some well known Hollywood actors, all at the peak of their careers and all of whom according to The Sunday Times of July 28th 2002 had BMIs over 30, and were therefore “obese:” Arnold Schwarzenegger, 257lb, 6ft 2ins = BMI 33; Tom Cruise, 201lb, 5ft 7ins = BMI 31.5; and Sylvester Stallone, 228lb, 5ft 9ins = BMI 33.7.
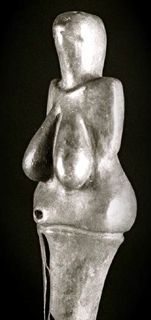
Iconic modern males may not seem directly relevant, and you can get round the problem by having different BMIs for males and females. Nevertheless, a prehistoric female icon like the Dolní Věstonice Venus, a figurine dating from 28,000 years ago and illustrated left, is clearly in the “obese” quadrant for BMI. However, her waist-hip ratio (WHR) is quite another matter. As I explained in a previous post, WHR correlates strongly with fat distribution in the body. And as this figurine also illustrates, oestrogens stimulate women to deposit fat on the buttocks, thighs and breasts. WHR is similar for the sexes before puberty, but afterwards women’s range from 0.67-0.8, whereas men’s go from 0.85-0.95. Risk of obesity-related diseases such as diabetes, hypertension and heart disease vary with WHR, so that it is also a good indicator of health in this respect. Indeed, higher WHR indicates increased risk of death in women independently of weight. And as I also noted in the earlier post, lower WHRs in women correlate with higher IQs in their children. Interestingly, this figurine has a WHR estimated to be 0.7, which is the value preferred by judges of both sexes viewing female body profiles with differing weights and WHRs. So, whatever her BMI, this Venus’s WHR is about right.
And as this supposed fertility fetish also suggests, fatness goes with fecundity: normal weight US women average 3.2 children, over-weight/obese 3.5. In the case of the Ache hunter-gatherers, the mean age at which women first gave birth was found to be the same as that at which they first reached mean weight for adult females in the population. Heavier women were also found to have more children, to have them more closely spaced, and to have children who survived better than did the offspring of lighter women. Since maternal investment in the developing foetus is principally in the form of nutrients, it is not surprising that it is the level of such nutrients stored in the mother's body—fat, in other words—which is critical to fertility. So sensitive is the female body to body weight variations that some women athletes can turn their sexual cycles on and off at will with just a three pound change in weight.
Even if restricted to populations as Keys intended, BMI is not as simple as it seems. The highest life expectancy in 2 million Norwegians was found in the “over-weight” part of the population, that is, those with BMI 26-28. The “ideally slim,” with BMI 18-20 had lower life expectancy than the “obese” with BMI 34-36, while being “under-weight” (BMI<18.5) was associated with more excess death than BMI 30-35.
When explaining this to students, I used to speculate that the reason could be that heavier weight might stand a person in better stead in the face of surgery or serious illness later in life, never dreaming that this is exactly what would happen to me. Radical cancer surgery reduced my weight by 25%, my BMI from an “obese” 30 to a “normal” 22, and took 6 inches off my waist. Had I started with an ideal BMI, I would have ended up dangerously underweight. Furthermore, I only managed to stabilize my weight by means of eating the "unhealthy" fatty, starchy, and sugary diet blamed for obesity.
A 10-year WHO study of 140,000 people in 38 countries on 4 continents in 2001 saw increases in BMI associated with decreases in high blood pressure and cholesterol, concluding: “These facts are hard to reconcile” with the conventional wisdom, particularly in view of the fact that predicted increases in mortality due to obesity have not occurred, and life expectancy continues to improve along with increasing average body weight in industrialized countries. Indeed, in 2006, 20 obesity experts were quoted concluding that evidence that slothful lifestyle and junk food contribute to obesity is “largely circumstantial,” while large-scale longitudinal studies of Californian women and Native American children have found no health gains or significant reductions in body fat due to “healthy diet.”
In the view of J. Eric Oliver quoted in Scientific American for June 2005:
a relatively small group of scientists and doctors, many directly funded by the weight-loss industry, have created an arbitrary and unscientific definition of weight and obesity. They have inflated claims and distorted statistics on the consequences of our growing weights, and they have largely ignored the complicated health realities associated with being fat.
How fat you normally are is a matter largely determined by your genes: BMI of adopted children resembles biological, not adoptive parents, and twin studies suggest 70% BMI heritability, with shared environment having little or no effect. Race/ethnicity is also a factor: in the US, Mexican-American women are 30% more likely than whites to be obese, and black women twice as likely.
Indeed, according to the thrifty gene theory, risk of type 2 diabetes and the “obesity” which often goes with it is an evolved factor to promote fat gain and efficient use of food in times of abundance, with survival value for periods of shortage. Lack of mass starvations in Europe since the 17th century could explain low incidence of diabetes among native Europeans thanks to selection against it, but the likelihood that the Pacific was peopled by the starved survivors of epic canoe voyages might explain why prevalence is so high among their descendants. Most notably, the incidence of this late onset disorder went from zero on the island of Nauru in 1952 to 41% in 2002, with two-thirds of all Nauruans over 55 being diabetic, and 70% being so over the age of 70 following the discovery of phosphates and the conversion of the islanders’ life-style to an affluent Western one (above left).
The Nauru story epitomizes the truth that it is a question of nurture via nature, not the reverse, as is so often asserted. Nauruans’ Western diet is indeed causing an epidemic of type 2 diabetes, but only because Nauruans are genetically predisposed to the disorder by way of being descended from founders who could put weight on to the point of being fat enough to survive starvation on canoes colonizing the Pacific.
Exactly the same is true of maternal “obesity” and risk of ASD. Modern life-styles and diet have unquestionably released more resources for development during gestation in many modern Western women, but this has been more to the benefit of the paternal genes in the foetus and placenta than to that of the maternal ones. As a result, a mother—no matter what her BMI—could righty blame a child’s paternal growth-enhancing genes for most of its eventual growth and associated risk of ASD: in other words, the genes for whom she is effectively providing the proverbial free lunch, thanks to the fact that only the mother pays the biological costs of gestation and lactation. And of course, because such genes as IGF2 are normally expressed only from the father's copy, it is hardly surprising that paternal obesity has also been linked to risk of ASD. Indeed, as the meta-analysis I am quoting points out, "studies also suggested that when adjusted for paternal and other confounding factors, the risk of autism in children with obese mothers was attenuated."
(With thanks to Amar Annus for bringing this to my attention, and to Randy Jirtle.)
References
Campos, P. 2004 'Why our fears about fat are misplaced', New Scientist (1 May 2004): 20-1.
Motluk, A. ‘Supersize surprise’, New Scientist, 4 November 2006, pp. 34-8.
Diamond, J. 2003 'The double puzzle of diabetes', Nature 423: 599-602.




