Health
Ain't Misbehaving? Self-Inflicted Illness
We blame the victim for failures of self-care.
Posted January 4, 2022 Reviewed by Michelle Quirk
Key points
- Difficult moral questions arise when we consider personal responsibility for maintaining our health.
- There is more to health than personal responsibility, including the environment, economics, and genetics, and causation is difficult to prove.
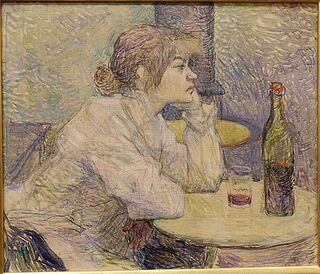
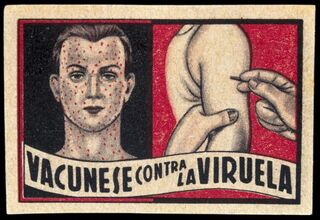
- Self-inflicted diseases due to alcoholism, drug abuse, obesity, and even vaccine refusal engender stigma and victim-blaming.
Should a patient with serious liver disease due to years of chronic alcoholism receive a new liver? What about a lung transplant for a three-pack-a-day smoker who continues to smoke? Or should a morbidly obese person qualify for bariatric surgery without complying with a regimen of diet and exercise?
Most relevantly, what about care for those who have refused vaccinations for COVID-19, potentially jeopardize those around them, and now require a respirator and months of ICU treatment to stay alive?
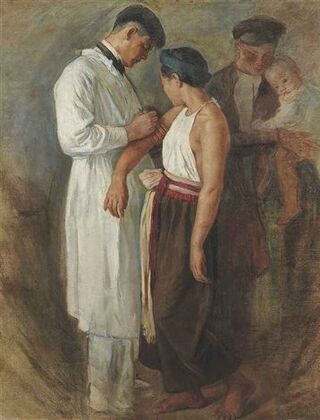
These are difficult moral questions that arise when we consider how much responsibility we have for our own health, particularly when our behavior affects those in the community and health care resources are finite.
“Germane to civil liberties and human rights is a right to be free from being harmed by others” (Terry, 2022). Not everyone, though, agrees on what is harmful.
The Internet, for example, is rife with pseudoscientific data accepted by those who oppose vaccination. The anti-vaxxers see themselves as "health advocates and crusaders," and, more dangerously, as “informed experts” (DiRusso and Stansberry, 2021).
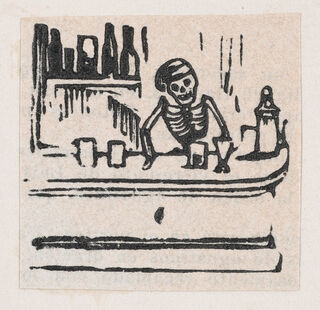
Some who challenge the anti-vaxxers, though, believe "certain failures of self-care," such as refusal to get vaccinated, fall into the “crimes against society" category that Fitzgerald described in the 1990s. After all, "society has to pay for their consequences,” wrote Fitzgerald, and "people owe it to society to stop misbehaving.” Illness, then, becomes evidence of this misbehavior, particularly when it comes to conditions of “self-abuse” (e.g., obesity, alcoholism, smoking, IV drug abuse, AIDS, or, now, even COVID-19). Many believe that those affected have brought it on themselves and deserve our condemnation.
“One man’s freedom in health is another man’s shackle in taxes and insurance premiums,” wrote physician John Knowles, then head of the Rockefeller Foundation (1977), who noted that health insurance is really “disease insurance.” Knowles believed that people had a “public duty” to preserve their own health since the costs of "individual irresponsibility in health" had become "prohibitive."

Using personal responsibility to ration health care is clearly controversial. Blaming the victim may place "unfair burdens" on those most vulnerable (Buyx, 2008), including the elderly, poor, disabled, mentally ill, or addicted, and it fails to recognize that there are multiple factors, including political, economic, and environmental, besides personal behavior, that may contribute to health (Allegrante and Green, 1981).
The notion of personal responsibility for health has a long history, even appearing in Hippocrates’s Regimen, and has surfaced periodically over the centuries (Reiser, 1985). Health care as a "social right" became popular in the 1970s with Medicare and Medicaid legislation (Reiser).
Some researchers believe a focus on personal responsibility has emerged more recently in response to a “growing disillusionment with the limits of medicine” as well as pressures to contain costs and growing self-help movements (Minkler, 1999). “Medical services as a means to maintain health have been grossly oversold” (Crawford, 1977).
Nowhere is this clearer than during our COVID-19 pandemic: “Medicine is permeated with ignorance” (Whooley and Barker, 2021). Furthermore, as the “illness experience” has moved online, the Internet has become “an information vending machine”; illness that was once “largely private and solitary” is "increasingly a public and collective experience” (Whooley and Barker).

Our understanding of disease, though, is fraught with uncertainty; its scientific basis changes over time (Fitzgerald). Obesity is a case in point: Even the concept of obesity as a disease remains controversial. Over the years, obesity has been considered a sin involving gluttony and sloth, an aesthetic crime, a failure of energy balance, an appropriate or inappropriate adaptation to an obesogenic environment, a genetic disorder, a psychological–behavioral disorder involving self-regulation or addiction, and even an example of body diversity (Karasu, 2014).
In a fascinating study, Allison and colleagues found that attitudes toward those with obesity are significantly influenced by the extent to which obesity is perceived as within a person's control: there is more tendency to stigmatize those with obesity when people believe obesity results from a person's behavior (Allison et al., 1991).
More recently, Ringel and Ditto replicated the findings of Allison et al.: The more people attributed obesity to behavior, the more disgusted they were and the more likely they were to discriminate against obese people. They were also more likely to view bariatric surgery as unnecessary or even as a "lazy method" to achieve weight loss, even when researchers explained that surgery still required considerable effort on the part of a patient (2019).
Friesen (2018) found that discussions of personal responsibility really reflect biases toward highly stigmatized behaviors. "Self-inflicted" diseases suffer from low "disease prestige" (Traina and Feiring, 2020). If responsibility really were taken into account, any dangerous job, hobby, or sport would have to come under scrutiny (Friesen).
Furthermore, our whole notion of cause and effect, including the concept of causal responsibility, is exceptionally difficult to substantiate (Buyx). Allison and colleagues, though, found (Cofield et al., 2010; Ejima et al., 2016) “inappropriate" use of causal language pervades research studies, particularly those in nutrition and obesity.

Despite difficulties in assigning causality or even determining responsibility (Friesen), the United Kingdom has proposed measures to restrict elective surgery for patients who smoke or are obese until they undergo a "health optimization process," a term straight out of Orwell, that calls for a time period for patients to change their behavior (Pillutla et al., 2018).
Clearly, behavioral change is difficult to maintain over time (Minkler). While self-inflicted diseases generate stigma and victim-blaming, though, limitations of medicine force society to demand we take at least some personal responsibility for our health.
References
1. Allegrante, J.P., Green, L.W. (1981). Sounding Board: When health policy becomes victim-blaming. The New England Journal of Medicine 305(25): 1528–1529.
2. Allison, D.B., Basile, V.C., Yuker, H.E. (1991). The measurement of attitudes toward and beliefs about obese persons. International Journal of Eating Disorders 10(5): 599–607.
3. Buyx, A.M. (2008). Personal responsibility for health as a rationing criterion: why we don’t like it and why maybe we should. Journal of Medical Ethics 34: 871–874.
4. Cofield, S.S., Corona, R.V., Allison, D.B. (2010). Use of causal language in observational studies of obesity and nutrition. Obesity Facts 3: 353–356.
5. Crawford R. (1977). You are dangerous to your health: the ideology and politics of victim blaming. International Journal of Health Services 7(4): 663–680.
6. DiRusso, C, Stansberry, K. (2021). Unvaxxed: a cultural study of the online anti-vaccination movement. Qualitative Health Research 0(0): 1–12.
7. Ejima, K. et al. (2016). Observational research rigour alone does not justify causal inference. European Journal of Clinical Investigation 46(12): 985–993.
8. Fitzgerald, F. (1994). The tyranny of health. The New England Journal of Medicine 331(3): 196–198.
9. Friesen, P. (2018). Personal responsibility within health policy: unethical and ineffective. Journal of Medical Ethics 44: 53–58.
10. Karasu, S.R. (2014). The obesities: an overview of convergent and divergent paradigms. American Journal of Lifestyle Medicine 10(2): 84–96.
11. Knowles, J.H. (1977). The responsibility of the individual. Daedalus 106(1): 57–80.
12. Minkler, M. (1999). Personal responsibility for health? A review of the arguments and the evidence at century’s end. Health Education & Behavior 26(1): 121–140.
13. Pillutla, V., Maslen, H., Savulescu J. (2018). Rationing elective surgery for smokers and obese patients: responsibility or prognosis? BMC Medical Ethics 19: 28–37.
14. Reiser, S.J. (1985). Responsibility for personal health: a historical perspective. The Journal of Medicine and Philosophy 10: 7–17.
15. Ringel, M.M., Ditto, P.H. (2019). The moralization of obesity. Social Science & Medicine 237: Article 112399: 1–10.
16. Terry, P.E. (2022). On the need for an association for vaccinated person’s rights (editorial). American Journal of Health Promotion 36(1): 13–17.
17. Traina, G., Feiring, E. (2020). "There is no such thing as getting sick justly or unjustly"—a qualitative study of clinicians’ beliefs on the relevance of personal responsibility as a basis for health prioritization. BMC Health Services Research 20: 497.
18. Whooley, O., Barker, K.K. (2021). Uncertain and under quarantine: toward a sociology of medical ignorance. Journal of Health and Social Behavior 62(3): 271–285.




