Appetite
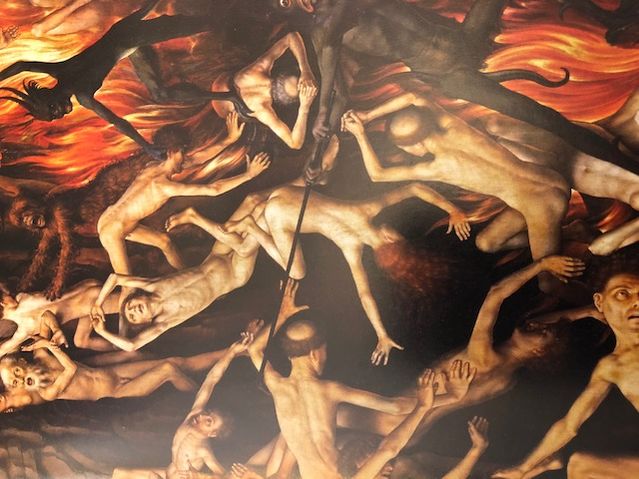
The "Disfiguring Mayhem" of Cancer Cachexia
Withering away: the deadly consequences of fatigue and emaciation.
Posted August 10, 2018

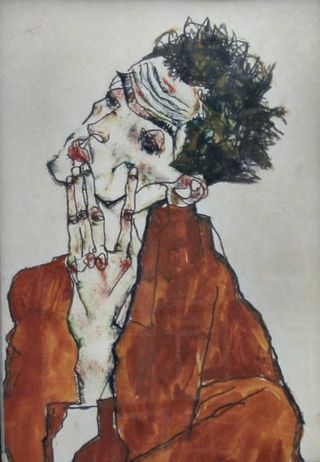
"I don't have a body. I am a body," wrote Christopher Hitchens, diagnosed with esophageal cancer and having lost 14 pounds that no amount of tube feeding could correct, in his final memoir, Mortality. (2014) Walking to the refrigerator became "like a forced march." He continued, "You lose weight but cancer is not interested in your flab. It wants your muscle." With ruthless brutality, his cancer gave him "gut-wringing nausea on an utterly empty stomach" and the "double-cross of feeling acute hunger while fearing even the scent of food." Likewise, Dr. Paul Kalanithi, neurosurgeon and himself dying of Stage IV lung cancer, wrote, in his book When Breath Becomes Air (2016), how he suffered from a "profound bone-weariness" after chemotherapy and felt "withered:" "I could see my bones against my skin, a living X-ray."

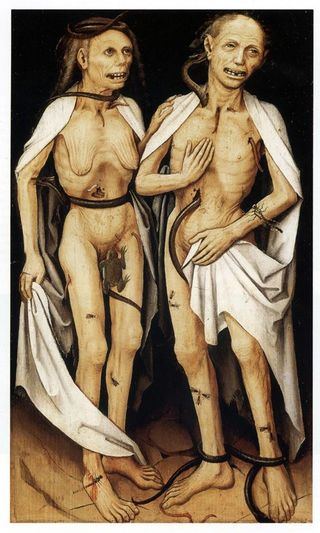
These are descriptions of cancer cachexia--from the Greek for "bad condition." Cachexia causes a wasting of the body and stems from an imbalance of the body's anabolic and catabolic processes. It can occur in other chronic, debilitating diseases such as AIDS, chronic obstructive pulmonary disease (COPD), and cardiac disease, (Penet and Bhujwalla, Cancer Journal, 2015) but is associated most commonly with advanced cancer, where it affects 60 to 80 percent of patients and is "directly implicated" in 20 percent of the "spectacularly wretched deaths" (Sontag, Illness as Metaphor, 1989) from cancer. (Vaitkus and Celi, Experimental Biology and Medicine, 2017) Half of all the cancer deaths worldwide—about 8.2 million a year—are attributed to cancers (e.g. pancreatic, esophageal, pulmonary, hepatic, colorectal) that are most often associated with cachexia. (Baracos et al, Nature Reviews, 2018) Almost any kind of cancer, though, can be associated with cachexia. (Vaitkus and Celi, 2017)
There have been many definitions of cachexia over the years, but the one commonly, but still not universally used now, was delineated by Fearon and colleagues (Lancet Oncology, 2011): a multifactorial syndrome defined by ongoing loss of skeletal muscle with or without accompanying loss of fat that cannot be reversed by conventional nutritional support and can lead to progressive functional impairment. Essentially, cachexia creates what some researchers have called metabolic mayhem. (Tsoli and Robertson, Trends in Endocrinology and Metabolism, 2013) With the accompanying fatigue and anorexia, i.e., reduced food intake, a patient can experience a dramatic decline, both physically and psychologically, in his or her quality of life. Several factors can lead to anorexia, including nausea, changes in taste and smell, GI obstruction, malabsorption, vomiting, diarrhea, effects of chemotherapy, and even anxiety and depression. (Ryan et al, Proceedings of the Nutrition Society, 2016) Furthermore, anorexia can be caused by substances released by the tumors, i.e., pro-inflammatory cytokines, sometimes referred to as "tumorkines" (Tsoli and Robertson, 2013), such as interleukin 1 or 6 and tumor necrosis factor alpha, among many others. Some tumors directly affect zinc metabolism, with accompanying negative effects on food intake. (Ezeoke and Morley, Journal of Cachexia, Sarcopenia, and Muscle, 2015)

Fearon et al (2011) noted that cachexia can occur on a continuum, and it represents "a spectrum of conditions." (Ryan et al, 2016) Sometimes, "substantial" unintentional weight loss occurs even before the diagnosis of cancer in a pre-cachexia syndrome, with early clinical and metabolic signs, including impaired glucose tolerance, anemia, and general inflammation. If refractory cachexia develops, there is often a life expectancy of less than 3 months. The mechanisms involved that lead to mortality include cardiac arrhythmia, electrolyte imbalances, respiratory difficulties due to muscle weakness, aspiration pneumonia, sepsis, etc. (Baracos et al, 2018)
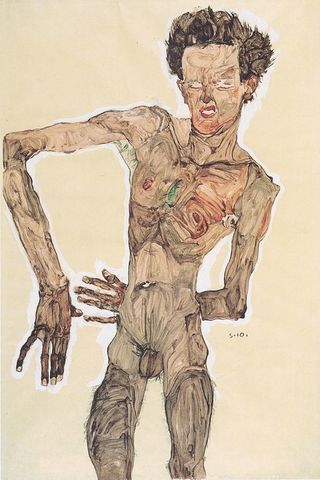
The risk of progression can vary from one patient to another (and some patients are genetically more resistant to developing cachexia than others), and can depend on the type of cancer, stage, time of diagnosis, body composition, presence of systemic inflammation, reduced food, particularly protein, intake, and even the gut microbiome. (Loumaye and Thissen, Clinical Biochemistry, 2017) Researchers question whether all cachexia is the same because cachexia can develop from disease-specific, treatment-specific, or tissue-specific mechanisms. (Kays et al, Journal of Cachexia, Sarcopenia, and Muscle, 2018) Other aspects associated with the diagnosis include an unintentional weight loss of greater than 5 percent within six months or a body mass index (BMI) of less than 20 kg/m.2 Fearon et al, 2011, though, emphasize that clinicians should not just focus on weight loss, but rather on sarcopenia, i.e., loss of muscle, with reduced muscle mass and loss of strength. Further, with the loss of muscle, patients are more susceptible to the toxic effects of treatment, with the possibility of being "overdosed."
Detecting cachexia, though, may be difficult because muscle mass can vary considerably across populations, and there is no biomarker (to date) that is highly specific for detecting skeletal muscle wasting. (Loumaye and Thissen, 2017) Furthermore, BMI is not a precise measure of body composition and does not measure muscle: people with the same BMI can have very different body compositions. (Caan et al, Cancer Research, 2018) Muscle can be assessed by CT or DXA (used to evaluate bone density) scans, but these can subject patients to additional radiation exposure. (Loumaye and Thissen, 2017)
Ironically, what also makes the diagnosis particularly challenging in recent years is that 40 to 60 percent of patients are overweight or obese at the time they are diagnosed with cancer. (Prado et al, Proceedings of the Nutrition Society, 2016; Schwarz et al, BMC Cancer, 2017) In fact, many cancers—perhaps between 15 to 45 percent—are considered directly related to obesity. (Ryan et al, 2016) As a result, patients can have "severe depletion" of skeletal muscle that remains undetected, and with this "upward shift" in BMI, the diagnosis of cachexia becomes much less clear. (Baracos et al, 2018) Further, those with increased adipose tissue may be at risk for chemotherapy toxicity because some drugs are lipophilic, with a longer elimination half-life. (Ryan et al, 2016)
The goal of treatment is to preserve muscle and stabilize weight. Early diagnosis and careful monitoring of weight are particularly important because unlike in starvation where increased food intake reverses the condition, cachexia is not completely reversible. (Schwarz et al, 2017) Patients often require "active nutritional management," including use of tube feeding and/or intravenous feeding, either by central or peripheral vein. (Baracos et al, 2018) Unfortunately, though, clinicians often don't know enough about specific nutritional requirements for cancer patients and know even less about those requirements for those who are also obese. (Ryan et al, 2016) An exercise regimen involving aerobic and resistance exercises is also recommended but clinicians appreciate that patients are often too debilitated to comply. (Baracos et al, 2018) Some orexigenic medications/drugs have been tried but there are no conclusive data. A recent scathing review of the use of the "hunger hormone" ghrelin found the research for outcomes relating to body weight and food intake of "very low quality," due to poor methodology, inadequate reporting of data, and small sample sizes. (Khatib et al, Cochrane Database of Systematic Reviews, 2018) Other medications that can be appetite stimulants have adverse effects, as for example, corticosteroids that can increase the risk of thromobembolism or even cause muscle atrophy. (Baracos et al, 2018)

Bottom line: There are still many unanswered questions about the complex mechanisms involved in cachexia. Diagnosis should be made as early as possible but is often made more difficult because there is no universally agreed upon definition nor any biomarkers specific to cachexia, and many patients diagnosed with cancer, ironically, are overweight or obese and have "cryptic cachexia." (Tsoli and Robertson, 2013) Cancer cachexia leaves the patient physically and psychologically debilitated as it creates its metabolic mayhem. To date, there are no evidence-based treatments.
Note: My title, Disfiguring Mayhem, comes from a quotation by Mark Twain, 1870, writing in a Virginia newspaper (and having nothing to do with cancer or cachexia.) Mayhem is from the root "to maim."