Psychosis
Psychosis Sucks!
Antipsychiatry and the romanticization of mental illness
Posted March 5, 2015
Earlier this year, Dr. Tanya Luhrmann, an anthropologist at Stanford University and author of Of Two Minds: The Growing Disorder in American Psychiatry created a few waves in a New York Times op-ed piece called “Redefining Mental Illness” [1]. In it, she talked up a “radically different vision of severe mental illness from the one held by most Americans, and indeed many American psychiatrists.” This purportedly new view of mental illness, she wrote, “rejects the centrality of diagnosis” embodied in “our current diagnostic system” (i.e. psychiatry’s DSM-5) in favor of a continuous view in which the dividing line between mental illness and normal experience isn’t so clear.
Dr. Luhrmann’s article provoked a spirited video response on medscape.com from Dr. Jeffrey Lieberman, past president of the American Psychiatric Association and current Chairman of Psychiatry at Columbia University, entitled “What Does the New York Times Have Against Psychiatry?” [2]. There he called Dr. Luhmann’s piece “an incredibly unscholarly, misinformed, confused—at worst, unhelpful, and at best, destructive—commentary that will add to the confusion about the diagnosis of mental illness, enhance the stigma, and may lead some patients to doubt the veracity of the diagnoses that they have been given and the treatments that they are receiving.” He went on to lament that his response had not been accepted for publication in the New York Times and asked, “Why would such a report be printed in a widely respected publication such as the New York Times?” and “What would give an anthropologist license to comment on something that is so disciplined, bound in evidence, and scientifically anchored?”
A few days later, Dr. Luhrmann, apparently pleased as if having prodded a grumpy old bear, placed a link to Dr. Lieberman’s article on her public Facebook page, with the headline “Well well. I must be doing something right.”
At the heart of this spat is a recently published monograph called “Understanding Psychosis and Schizophrenia: Why People Sometimes Hear Voices, Believe Things That Others Find Strange, or Appear Out of Touch With Reality …and What Can Help” [3]. It was this 180-page document, put out by the British Psychological Society (BPS), that Dr. Luhrmann was speaking of when she discussed a new way of looking at mental illness and psychosis in particular. As she described, the report advances the view that psychotic symptoms should be conceptualized on a continuum, noting that some “normal” people have experiences such as voice-hearing, which can even be valued by some individuals and cultures. It goes on to argue against the prevailing medical model of psychosis on the basis that many people with psychotic experiences prefer not to think of themselves as mentally ill and the observation that life experiences such as trauma, beyond biological factors like genetics, seem to contribute to the development of experiences such as voice-hearing.
Perhaps unsurprisingly, reviews of the BPS publication have for the most part been divided between psychiatrists and non-psychiatrists. On one side, a press release calls the report “ground-breaking,” a contributing author promotes it as “radical” and “revolutionary,” and Dr. Luhrmann touts it as “remarkable.” On the other side, Dr. Lieberman describes the report’s normalization of psychotic symptoms as “preposterous… at best, phenomenologic relativism, and at worst, simply conflating symptoms with a disorder or a disease.” Several other psychiatrists have commented on the report’s overreaching claims about the efficacy of psychotherapy as compared to antipsychotic medication (see here and a debate with one of the BPS report authors here). And it’s not only psychiatrists who are objecting—Dr. James Coyne, a psychologist, has offered a particularly critical analysis of the BPS report, noting that it lacks credibility by offering a self-serving anecdotal, rather than evidence-based, account of psychosis.
Given this sharp divide, can the BPS report be viewed from a sensible middle-ground?
Of course, I’m a psychiatrist myself, so my answer may be predictable, but if nothing else perhaps I can clarify why Dr. Lieberman, along with many other psychiatrists, have been critical of the report.
Before I do, let’s begin by acknowledging that the authors of the BPS report are an amalgam of well-respected clinical researchers, most of whom are psychologists from the UK. The subjective experience of patients with psychosis and the value of making fine distinctions between different types of seemingly similar experiences such as “hearing voices” have been relatively neglected in American psychiatric research, such that the work being done in the UK by these authors has been an important font of knowledge over the past few decades. See, for example, this recent special issue of Schizophrenia Bulletin devoted to hallucinations, to which many of the BPS report authors contributed. It represents a “state of the art” summary of what we know about voice-hearing, both in those with mental illness as well as those without.
Next, let’s make clear that the BPS report itself includes plenty of information with which nearly all psychiatrists and any other mental health clinicians would agree. Each individual’s experiences are unique. Psychotherapy can be helpful for those with psychosis. Medications have side effects and don’t always work. Clinicians should work collaboratively with patients. We should all work to destigmatize mental illness. No arguments there.
Then there’s the core premise of the report, that psychotic symptoms span a continuum of severity, with some experiences failing to meet the necessary threshold for a mental disorder. My own work has covered this issue in some detail, including this very blog, Psych Unseen, which aims to address “the psychiatry of everyday life”—that is, the myriad quirks of normal human behavior that parallels or has potential overlap with psychopathology.
In 2010, I wrote a paper called “Hallucinations in Non-Psychotic Disorders: Towards a Differential Diagnosis of ‘Hearing Voices’” in which I discussed how voice-hearing can be present in those without mental illness as well as those with conditions other than psychotic disorders [4]. I described the continuum or “spectrum” model of voice-hearing that is supported in the BPS report and suggested that:
“Similar to the likening of psychosis to fever, auditory hallucinations [AH] might be best compared to coughs – normal and even functional experiences that can occur spontaneously or in response to environmental stimulation, reflect or be part of a larger clinical disorder, or be malingered. As with coughs, clinicians and researchers ought to focus on recognizing what makes AH clinically relevant, distressing, or functionally impairing. Candidate variables include frequency, preoccupation, insight, control, and perceived omnipotence, to name a few. Depending on these factors, potential treatment strategies might include watchful waiting, palliative therapies directed at the “symptom” itself, or targeting the larger, underlying disease.”
In another 2010 paper entitled “Nonantipsychotic Therapy of Monosymptomatic Auditory Hallucinations,” I highlighted the potential inaccuracy of a schizophrenia diagnosis among hospitalized voice-hearers and noted that voice-hearing can sometimes improve without need of antipsychotic medications [5].
With all this agreement, what then, do I and other psychiatrists find troubling about the BPS report?
Dr. Allan Frances, the chairperson of the Taskforce on DSM-IV and author of the Psychology Today blogs “Saving Normal” and “DSM in Distress,” recently authored a pro- and con- debate with the BPS report’s editor, psychologist Anne Cooke, in which he argued that that in failing to distinguish between clear-cut psychosis and more benign experiences, the report runs the risk of providing potentially dangerous advice to those with serious illness [6]. Likewise, my colleague Dr. Ronald Pies, Editor in Chief Emeritus of Psychiatric Times, has expressed concerned that it “trivializes the very real suffering of those with psychosis” [7].
What they’re referring to is that the BPS report, which contains innumerable quotations from those with psychotic symptoms, has a consumer-targeted feel and an overall tone that’s casual almost to the point of being sing-song. Reading in between the lines of what Dr. Pies calls the “feel-good generalities,” it promotes a main message that people need not accept medical models of psychosis and might do just as well to “find meaning” in their symptoms, embrace “psychological therapies,” and opt out of taking medication. In other words, if you don’t want to think of yourself as mentally ill, then don’t. If you don’t want to accept recommendations for medications, then don’t.
To a psychiatrist who treats people with serious mental illness, this sounds like dangerous advice. One of the biggest challenges of working with patients with psychotic disorders is getting them to accept their diagnosis and to engage in treatment, whether pharmacotherapy or psychotherapy. The very definition of delusional thinking, one of the hallmarks of psychosis, includes the belief that there’s nothing wrong and that one doesn’t need treatment. This lack of insight is one of the most common barriers to recovery. Even patients who do respond well to medications often go on to relapse time and again when they inevitably stop taking them and are “lost to follow-up” due to beliefs that they’re not ill or that treatment is no longer needed. The BPS report seems to reinforce such beliefs.
Dr. Lieberman chalks up the Times’ publication of Dr. Lurhmann’s article to “anti-psychiatry,” noting that “psychiatry has the dubious distinction of being the only medical specialty with an anti-movement.” But psychiatry isn’t really the only medical discipline with an anti-movement. The fact is, there are plenty of people who have spoken out about their bad experiences across all of western medicine. There are plenty of people who eschew the care of physicians in favor of seeking out unproven alternative interventions. There are plenty of people who don’t want to be thought of as “sick.”
But to those of us within medicine, this kind of thinking sounds perilous when juxtaposed against recent stories of people dying from leukemia because they opted for naturopathic remedies, or politicians saying that cancer is a fungus that can be treated with baking soda, or the emergence of measles in the midst of the current anti-vaccine movement. This is not to say that western medicine is perfect and never associated with unfortunate outcomes, only that adopting a blanket opposition to medical care is ill-advised when one has a serious medical condition. And the same is true for psychiatry.
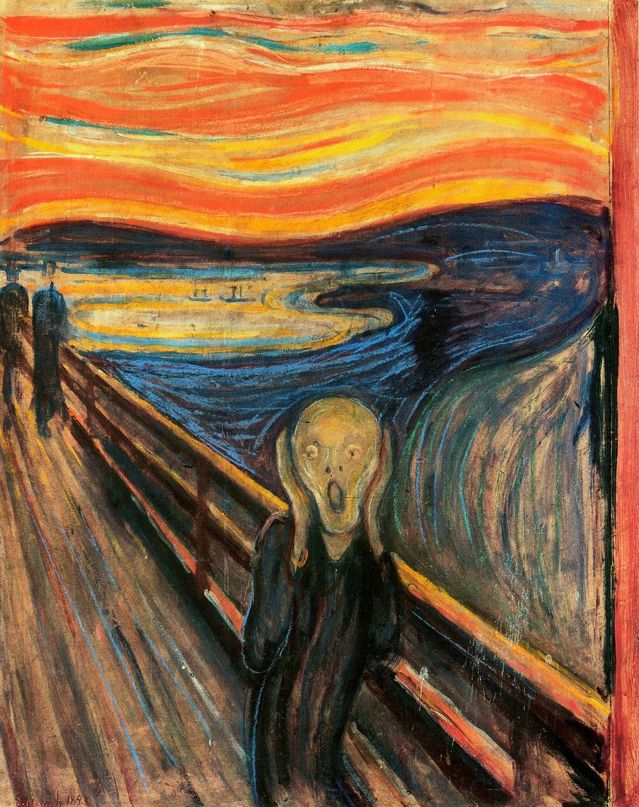
Viewed from this perspective, the BPS report goes beyond its well-intended attempt to destigmatize psychosis, treading into the territory of romanticizing it. It talks of the positive aspects of psychosis, the historical reverence of psychotic symptoms in shamanistic cultures, and a potential link between psychosis and creativity. Again, that sounds good, but to one experiencing a psychotic disorder, there are few upsides. Psychotic disorders are by definition associated with impairment, not benefits. And sadly, while there is a link between creativity and bipolar disorder, the creative spark is all too often destroyed among those with schizophrenia. We have a great need to destigmatize mental illness and a long way to go, but decreasing stigma doesn’t mean that the pathway to health lies in pretending that mental illness is no big deal, or as the BPS repeatedly says, a “dangerous gift.”
Contrast the underlying message of the BPS report with a major public health campaign in Canada called Psychosis Sucks! This effort, launched in 2003, aims to raise awareness about psychosis among young people who may be experiencing new onset symptoms so that they’ll be encouraged to seek help. Similarly, the ReachOut Psychosis campaign’s message—“psychosis sucks if there’s nobody around to catch you”—is designed to engage those struggling with psychosis in order to maximize chances for recovery. These public health efforts make clear that psychosis is a disturbing and distressing experience and that delaying treatment has been associated with poorer outcomes. There’s no attempt to whitewash mental illness. Ultimately, destigmatizating mental illness is about public acceptance and improving treatment, not about suggesting that adopting a non-illness view of psychosis is an intervention in and of itself.
There’s a crucial point that seems to have been missed in the BPS’s promotion of the continuum model of psychosis. Like visible light, symptoms of mental illness are best thought of as both particle and wave. In other words, psychotic experiences seem to be distributed on a continuum of severity that spans from normal to mentally ill, but a key purpose of the DSM is to set an actual threshold to define what is pathological. For psychiatric disorders, that threshold is defined by a constellation of symptoms that are associated with distress or impaired functioning. As the BPS report suggests, symptoms that aren’t associated with distress of impaired functioning aren’t symptoms at all. But that’s not a new or radical concept—it’s inherent to the concept of mental disorder that’s made clear in the DSM. For example, there is no “hallucination disorder” that describes someone who hears voices but is not in distress and is doing just fine in terms of function. But just because psychotic experiences aren’t always symptoms of mental illness, doesn’t mean that psychosis is never a symptom, as my cough analogy makes clear (and incidentally, just because a symptom is a reaction to something doesn’t mean it’s not appropriate to call it a medical illness, as with chronic bronchitis due to smoking). Schizophrenia, which the BPS report includes in its title, is a psychiatric syndrome – a grouping of different psychotic symptoms that are by definition associated with significant suffering.
Based on their valuable contributions to research on voice-hearing, the BPS report authors would have been on firmer ground if they’d steered clear of schizophrenia and instead confined themselves to the phenomenon of auditory hallucinations. Had they done so, they ought to have also mentioned that the continuum model of auditory hallucinations is but one theory. In a brief paper I wrote in 2009 called “Naming Names: Auditory Hallucinations, Inner Speech, and Source Monitoring,” I highlighted the potential heterogeneity of experiences that are often lumped together under the generic heading of voice-hearing [8]. This heterogeneity supports an alternative view of voice-hearing not as a continuum (in which all voice-hearing is lumped together), but as a variety of fundamentally different brain processes (in which efforts should be directed at splitting disparate experiences apart from each other in terms of understanding their cause and proper intervention). According to this "splitting model," it’s possible that the experiences of people without mental illness who hear or even enjoy voice-hearing might be experiencing something altogether different that someone who is mentally ill and in distress. In fact, the work of some of the BPS authors, summarized in the special issue of Schizophrenia Bulletin that I mentioned above, addresses this very point. Distressing voices experienced by those that seek help are more negative in terms of content, have greater frequency and duration, impair functioning, and are associated with lower degrees of control and later onset in life [9]. If it’s true that voice-hearing in the context of mental illness is a different experience altogether than voice-hearing experienced by those who are normal, then the BPS report’s efforts to normalize psychosis across the board may be even further off base.
While the BPS report claims to offer a revolutionary new way of looking at psychosis, the truth is there’s little new about the idea. A century ago, modern psychiatry began with Freud’s psychoanalytic theories that posited that mental illness, including psychosis, was a reaction to life experiences. Such theories have been largely abandoned in the context of schizophrenia due to lack of empirical support. In the 1960s, UK psychiatrist Dr. R.D. Laing, drawing on his premise that insanity is a perfectly rational response to an insane world, created a group home for people with schizophrenia called Archway Community where residents were free to come and go as they pleased and antipsychotic medications were optional. Similar programs later emerged in the US, embodied in the Soteria Movement led by Dr. Loren Mosher starting in the 1970s. Earlier in my career, the idea of this kind of environment that intended to remove the stigma of mental illness and promote autonomy had a lot of appeal. Then, some years later, I watched Peter Robinson’s 1972 documentary film “Asylum” (not to be confused with the horror B-movie starring Peter Cushing released that same year) that followed the residents of Laing’s Archway Community over 6 weeks. What I saw (see a clip of the movie yourself here) wasn’t liberating, empowering, or evidence of recovery outside of the medial model. It was misery in the midst of chaos.
So it is with psychosis, at least in the form that’s associated with help seeking and mental illnesses such as schizophrenia. To psychiatrists who have worked with this kind of psychosis, the BPS report, with all of its sunny optimism, reads like a retread of misguided ideas and a whitewash of the harsh reality that is psychosis.
Psychologist Dr. James Coyne has noted that the many quotations included in the BPS report seem to have come from those who aren’t “service users,” that is, patients in treatment. As a counterpoint to that “cherry-picking,” I’ll close with a few quotations from young people, some of whom acknowledge having psychiatric disorders themselves, who have spoken out against the recent romanticization of mental illness in popular culture.
“The idea that mental illnesses are "beautiful" is something that bothers me immensely. …The glorification and romanticization of mental illnesses needs to stop because it is promoting pain. It is not cute or romantic to be suffering from a mental illness; it is painful. Anyone who is or has suffered from a mental illness will not sit there and tell you that it helped them find their soulmate or that it was fun, they’ll tell you that it was one of the most miserable times in their lives and that it is not something that they would wish on their worst enemy.” [10]
References
1. Luhrmann TM. Redefining Mental Illness. New York Times. Jan 17, 2015.
http://www.nytimes.com/2015/01/18/opinion/sunday/t-m-luhrmann-redefinin…
2. Lieberman JA. What Does the New York Times Have Against Psychiatry? Medscape. Feb 18, 2015.
http://www.medscape.com/viewarticle/838764
3. Cooke A, ed; British Psychological Society Division of Clinical Psychology. Understanding Psychosis and Schizophrenia: Why people sometimes hear voices, believe things that others find strange, or appear out of touch with reality, and what can help. London: British Psychological Society, 2014.
http://www.bps.org.uk/networks-and-communities/member-microsite/divisio…
4. Pierre JM. Hallucinations in Non-Psychotic Disorders. Harvard Review of Psychiatry 2010; 18:22-35.
http://journals.lww.com/hrpjournal/Abstract/2010/01000/Hallucinations_i…
5. Pierre JM. Nonantipsychotic Therapy of Monosymptomatic Auditory Hallucinations. Biological Psychiatry 2010; 68:e33-34.
http://www.sciencedirect.com/science/article/pii/S0006322310004208
6. Frances A. Pro and Con: The British Psychological Society Report on Psychosis. Couch in Crisis, Psychology Today Blog, December 19, 2014.
https://www.psychologytoday.com/blog/saving-normal/201412/procon-britis…
7. Pies R. Trivializing the Suffering of Psychosis: How the British Psychological Society’s Report Fails Our Sickest Patients. psychcentral.com
http://pro.psychcentral.com/trivializing-the-suffering-of-psychosis-how…
8. Pierre JM. Naming names: auditory hallucinations, inner speech, and source monitoring. Psychological Medicine 2009; 39:1578-1579.
http://journals.cambridge.org/action/displayAbstract?fromPage=online&ai…
9. Johns LC, Kompus K, Connell M et al. Auditory Verbal Hallucinations in Persons With and Without a Need for Care. Schizophrenia Bulletin 2014; 40 (suppl 4):S255-S264.
10. Ross K. The glorification of mental illnesses. May 1, 2014.
http://www.honestyforbreakfast.com/the-glorification-of-mental-illnesses
11. Hartman S. We need to stop romaticizing mental illness. December 27, 2013.
http://thoughtcatalog.com/sarah-hartman/2013/12/we-need-to-stop-romanti…
12. Low97. Stop romanticizing mental illness.
http://www.teenink.com/opinion/pop_culture_trends/article/633263/Stop-R…




