Depression
The Relationship Between Inflammation and Depression
Research has shown that inflammation plays a crucial role in depression.
Posted September 4, 2020 Reviewed by Kaja Perina
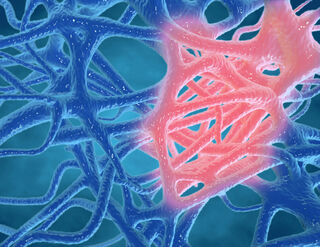
Research has shown that inflammation plays a crucial role in the development of depression. The inflammatory process in the body is a critical response to fighting off infections, but over time, it has also been linked to the development of depression.
When the body goes to war to fight off infection
Individuals who have higher levels of a specific inflammatory marker known as C-reactive protein (CRP) are at a higher risk of developing depression within five years. When bacteria, viruses, and parasites invade the body, the immune system recruits white blood cells, cytokines, and proteins to fight off the unwelcome invaders. The immune system works to mark certain areas as injured as a way to bring more attention to this area.
During this battle, the body will often show signs of illness and infection before it begins to recover. Acute inflammation can last from hours to days, whereas chronic inflammation can last for many years. Over time, chronic inflammation begins to break down the body, resulting in weakness and fatigue, which can also contribute to the development of depression.
Taking a look at the research
When individuals are injected with inflammatory markers, such as CRP protein and interferon (IFN-alpha), they tend to show higher rates of depressive symptoms compared to the control individuals who were not injected with inflammatory markers. Inflammation stresses the body, and as a result, many individuals will feel a lack of pleasure, experience sleep disturbances, and social withdrawal, and will notice impairments in their cognitive abilities. Individuals who do not respond to anti-depressants are known to have treatment-resistant depression and often show higher levels of inflammatory markers in their bodies.
Environmental stressors can cause inflammation
Stressful environmental triggers, such as poverty, abuse, and trauma, all contribute to the development of inflammation in the body. When the body is stressed, from either physical illness or a host of environmental stressors, it wants to fight off the “attackers” and, as a result, gives off an inflammatory reaction, increasing the risk for the development of depression.
The link between autoimmune disorders and depression
Autoimmune diseases are chronic inflammatory disorders that produce invaders known as antibodies that attack normal, healthy body tissues. In other words, the body attacks itself, creating an inflammatory reaction. Common autoimmune disorders include rheumatoid arthritis and lupus, and individuals with these chronic illnesses are more prone to the development of depression.
Experts believe that although the inflammatory process plays a role in the development of depressive-like symptoms, individuals with autoimmune disorders are more at risk for depression because these chronic diseases can take a toll on the individual’s lifestyle and well-being. Many individuals with autoimmune disorders experience pain and stiffness in the body, inhibiting them from enjoying many of the hobbies they love. Fatigue, an underlying symptom of depression, is also a common symptom seen in many autoimmune disorders. As a result, individuals who have an autoimmune disorder are at an even higher likelihood of developing depression, because they have a chronic disease, and they have an increase in inflammatory markers.
Looking towards the future
There is still much to be learned about the relationship between inflammation and depression, as researchers have only begun to scratch the surface. Current research is being performed to target inflammatory markers and prevent them from being active in the body to inhibit the downstream effects on neurotransmitters and brain circuits in hopes of preventing depression.
If you or someone you know is currently battling depression, it may be wise to speak to your therapist or health care provider about any underlying chronic inflammatory disorders that could be triggering the depression. Arthritis, gout, and lupus are just a few inflammatory disorders that can be triggers for depression, and often treating the underlying medical illness can play a huge role in managing the depression.


