Addiction
A Parallel Recovery: Families Healing From Addiction
Families and loved ones should heal in tandem to ensure a successful recovery.
Posted August 25, 2023 Reviewed by Ray Parker
Key points
- Families both affect and are affected by loved ones who struggle with substance abuse disorders.
- Parents with substance abuse disorders can harm kids' mental and physical health.
- A well-rounded approach to family care involves education, clinical interventions, and peer-driven support.
By Anthony Nave LICSW, LADC, ICAADC

A common saying at our treatment center is that we all know a loved one, either a friend or family member, who struggles with addiction. Provisional data from the Centers for Disease Control and Prevention (CDC) for 2022 is predicting another year of over 100,000 overdose deaths from drugs in the United States.
That is a lot of friends and family left behind to grieve the loss of what could have been, and the memories of what once was (CDC, 2023). Too often, we hear loved ones try to explain the torment they feel as they sit home wondering if today is “the day” their spouse, child, parent, sibling, or friend does not come back home, or the day they find their loved one unresponsive.
The impact on the well-being of friends and family is daunting to describe and quantify. In the ongoing effort to improve treatment for substance use disorders (SUDs), the health of family and friends cannot be forgotten as agencies work to perfect an effective integrated care model.
But I’m Not the One Who Is Sick
Families often give everything of themselves to help get a loved one into treatment. There can be, however, a mix of relief and fear when that loved one actually admits to treatment. In the first phone call from the therapist or doctor, families are anxiously waiting for an update on the well-being and progress of their family members.
What tends to immediately follow is families asking how they can further help; the last thing most want to hear is that they should start working on themselves. More often than not, I hear, “But I’m not the one who is sick.”
The Substance Abuse and Mental Health Services Administration (SAMHSA) provides much research and information on best evidenced-based practices for substance use disorder treatment and family therapy. A key point to understand is that families are both affected and are affected by loved ones who struggle with SUDs. The family and/or friend system has its own personality, just as much as the individual members who are a part of the family.
The system as a whole will adjust to each action by each member to try and maintain “homeostasis” to keep the family unit safe (SAMHSA, 2020). When a member of the family struggles with addiction, the family is in crisis and adjusts to help stabilize the unit as a whole and for each member.
This process is both universal and unique to each family and will shape the mood and behaviors of everyone in that family.
During treatment, an individual works with the clinical team to help soothe their fight, flight, and/or freeze response and progress toward sobriety. Parallel to that person's recovery, their family members need time and support to heal from the crisis too, and to nurture their own individual recovery, as well as the family system’s recovery. If the family does not work on themselves, it limits the chances of their loved one maintaining long-term recovery when they leave treatment (CDC, 2023).
How Are Family Members Impacted by a Loved One’s Addiction?
Research has found that 14 percent of children by age 17 have experience with household members who struggle with substance problems, and it is the second most commonly reported adverse childhood experience. Children living in a home with those with substance abuse disorders manifest a range of negative mental and physical side effects.
These children are more likely to have poor health, activity limitations, and chronic school absences than other children, and are two to four times more likely to develop mental health disorders, such as major depressive disorder, generalized anxiety disorder, post-traumatic stress disorder (PTSD), and SUD’s of their own (Turney & Olsen, 2019; Daley, 2013; Lander, Howsare, & Byrne, 2013).
The impact is not limited to children in the families but also includes adult members of the family as well. Studies have shown that family members of loved ones struggling with SUD are nearly 30 percent more likely to develop mental health disorders of their own, including PTSD, generalized anxiety disorder, and/or major depressive disorder.
Ongoing research shows the negative genetic impact SUD will have on future generations of the family, and scholars continue to share more insight on the impact of intergenerational trauma. The experience of living with and trying to care for family members, or friends who struggle with addiction, is traumatic and necessitates each family member having their own space to heal from the situation. When each family member invests in their own healing, the entire unit together is better prepared for the long recovery road ahead.
The Evolution of Addiction Treatment for Families
By the 1980s, specialized family SUD treatment programs were available often using Virginia Satir’s communication family model, and programs even began to develop support for the different subsystems of each family: couples, parent-to-young children, parent-to-adult children, siblings, and more combinations.
However, this new approach to family care did not make it far. In the 1990s, limited funding and managed care requirements for shorter treatment lengths negatively impacted the development of more involved services for integrated family treatment in SUD. Since then, a culture of viewing family services as an ancillary service has continued to be a barrier to getting more robust family programming, and a full continuum of care, despite the known positive effects they have on successful client outcomes (SAMHSA, 2020).
As of 2017, there has been more research and greater advocacy by scholars to resume and strengthen family treatment within SUD programs. Different treatment agencies have done well to develop a full continuum of services that includes, detox, residential, outpatient, recovery coaching, and community support services, to help individual clients achieve the goal of long-term recovery. It is now time to replicate a similar model of services for the family unit and its members for their own parallel recovery.
What Does the Parallel Process Look Like?
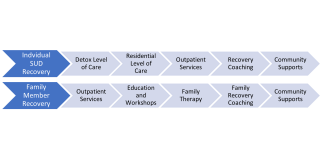
As a client starts their treatment journey at an inpatient level of care, their family and loved ones should simultaneously begin their own journey at an outpatient treatment and/or community support level to heal from their personal trauma and grief (SAMHSA, 2020). Family care for individuals with addicted loved ones needs to involve a combination of education, clinical treatment, and peer support. Everyone’s experience with SUD is different, so each family member’s treatment plan will vary.
Healthcare providers should use clinical interventions and modalities to heal symptoms of mood disorders and trauma through individual therapy, group therapy, family therapy, and medication management. By educating families on substance use disorders, they can be more empathetic and understanding of each family member's experience including their own.
Moreover, teaching individuals how to use positive communication skills to express emotions openly without resorting to hostility or blame is important to foster change. Through structured treatment, families can learn to identify behaviors sparked by fight, flight, and freeze responses that may perpetuate their loved one’s addiction and replace them with positive ones (SAMHSA, 2020).
What We Can Do
Viewing the family as a complex system helps us to recognize that what happens to one family member impacts the other. This feedback loop continues for both negative and positive experiences (SAMHSA, 2020; Lander, Howsare, & Byrne, 2013). Addiction is a family struggle, and therefore healing also is a family recovery process.
I often use the example of music when working with families to explain this process: We all need time to understand and learn how to play our own instrument before being able to join a larger band, and then learn how to play and make new music together.
Through treatment, workshops, and community resources for both client and family, we increase positive treatment outcomes and greater lasting change. Building a more robust parallel process of recovery for the individual client struggling with SUD and for their support network should be the standard for treatment agencies moving into the future.
Anthony Nave is an Internationally Certified Advanced Alcohol and Drug Counselor and Licensed Clinical Social Worker, who holds master’s degrees in Educational Psychology and Clinical Social Work. He is advanced certified in Eye Movement Desensitization and Reprocessing (EMDR) and is an EMDR Consultant. At Mountainside, he oversees clinical programming for the full continuum of care and incorporates interpersonal neurobiology and a trauma-responsive framework into treatment and supervision.
References
Centers for Disease Control and Prevention. (2023, May 18). NCHS: A Block of the National Center for Health Statistics. Retrieved July 23, 2023, from Centers for Disease Contorl and Prevention: https://blogs.cdc.gov/nchs/2023/05/18/7365/#:~:text=The%20only%20state%….
Daley, D. C. (2013, December). Family and Social Aspects of Substance Use Disorders and Treatment. J Food and Drug Anal., 21(4), S73-76. Retrieved July 23, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4158844/pdf/nihms599625.pdf
Lander, L., Howsare, J., & Byrne, M. (2013). The Impact of Substance Use Disorders on Families and Children: Theory to Practice. Soical Work Public Helath, 28(0), 194-205. Retrieved July 23, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3725219/pdf/nihms-496858.p…
Substance Abuse and Mental Health Services Administration. (2020). TIP 39: Substance Use Disorder Treatment and Family Therapy. Rockville, MD: SAMHSA. Retrieved July 23, 2023, from https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_Download/PE…
Turney, K., & Olsen, A. (2019). Household Member Substance Problems and Chlidren's Health in the United States. Elsevier: SSM - Population Helath, 7, 1-8. Retrieved July 23, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6517526/pdf/main.pdf




