Loneliness
Neurodegenerative Diseases, Novel Treatments
Old-school scientists may be stuck in the past.
Posted October 3, 2022 Reviewed by Gary Drevitch
Saskia Sivananthan, chief research officer at the Alzheimer Society of Canada, said recently that if not much changes to the current trends, the number of people with dementia and the number of people caring for them “is going to be enormous. By investing in addressing modifiable risk factors that improve brain health, we can start changing and shifting some of those numbers down.”
Don’t bet on it. Unfortunately, the experts at the ASC appear to speak only to like-minded old-school scientists largely unaware of the research on neurodegenerative disorders being conducted outside their bubble. According to the Alzheimer Society report, "Navigating the Path Forward for Dementia in Canada," “Certain risk factors like age and genetics are not modifiable.” While we all age, though, how we age is modifiable. We all know people who look and act 10 years younger than their chronological age and vice versa. Being active, having many interests, eating a proper diet, sleeping well, visiting your doctor for yearly check-ups, and not neglecting your oral hygiene are just some of the things we can all do to age well.
There is also some really exciting new research about rejuvenation. A study from the University of California-San Francisco showed that exposure of an aged animal to young blood can counteract and reverse pre-existing effects of brain aging by rejuvenating synaptic plasticity and improving cognitive function. This reminds me of the grotesque practice most commonly attributed to the historical figure of Elizabeth Bathory, a Hungarian countess and serial killer who lived from 1560 to 1614. Bathory believed that she could maintain eternal youth and beauty by bathing in the blood of virgins. Macabre, yes, but perhaps she was onto something?
Tal Iram, a young neuroscientist at Stanford University, infused, instead of blood, cerebrospinal fluid taken from young mice into old mice. For comparison, a separate group of old mice was infused with artificial cerebrospinal fluid. A few weeks later, the mice were exposed to cues — a tone and a flashing light — that they had earlier learned to associate with shocks to their feet. The animals that had received the young cerebrospinal fluid infusion tended to freeze for longer, suggesting that they had preserved stronger memories of the original foot shock.
The ASC report mentions social isolation as a risk factor, but does not discuss the connection between social isolation and the bacteria in our guts, commonly referred to as the gut microbiome, a focus of much research all over the globe. For example, scientists from University of California-La Jolla found that loneliness was associated with a lack of diversity in the gut microbiome. On the other hand, wisdom and compassion were associated with a diverse microbiome. Conversely, the researchers said that social support, compassion, and wisdom might confer protection against loneliness-related instability of the gut microbiome. The relationship between loneliness and microbial diversity was particularly strong in older adults.
Healthy, diverse gut microflora may buffer the negative effects of chronic stress or help shape social behaviors that promote either wisdom or loneliness. It is possible that loneliness may result in decreased stability of the gut microbiome and, consequently, reduced resistance and resilience to stress-related disruptions, leading to inflammation and disease.
Other surprising new research from Stanford shows that the buildup of neurofibrillary tangles of tau protein inside neurons in Alzheimer’s, Parkinson’s, and other brain diseases, which has been assumed to be the primary culprit, actually occurs in all aging cells, not just brain cells. Protein aggregation may be a universal phenomenon in aging cells and could be involved in many more diseases of aging than was suspected. Their discovery points to a new way of thinking about what goes wrong in cells as they age and, potentially, to new ways of preventing some unwelcome consequences of aging.
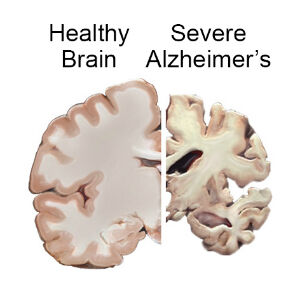
In the Alzheimer’s brain, abnormal levels of beta-amyloid protein, a naturally occurring protein, clump together to form plaques that collect between neurons and disrupt cell function. Pharmaceutical companies and neuroscientists have spent millions of hours and billions of dollars trying to clear the brain of these amyloid plaques.
Now a new study in the journal PLOS Biology, by John Mamo of Curtin University in Bentley, Australia, found that amyloid protein made in the liver, when transported to the brain, may be a significant contributor to neurodegeneration in the brain. Consequently, it seems logical to assume that the liver may play an important role in the onset or progression of the disease. Has anyone at the Alzheimer Society heard about this?
The "Navigating the Path Forward for Dementia in Canada" report advises us to get six-to-eight hours of quality sleep at night. Good advice. But what if you can’t? A majority of elderly people suffer from insomnia. The reason may be hiding in their gut. Diana Rogulja, an assistant professor of neurobiology at Harvard Medical School, recently discovered how sleep deprivation causes death in fruit flies and mice. Lethal changes occur not in the brain but in the gut by way of a preponderance of reactive oxygen species (ROS), free radicals. If ROS are not swept up by antioxidant enzymes, they may cause damage to DNA, RNA, and proteins, and may lead to cell death.
In conclusion, it appears that there are many avenues open to improve the lives of people suffering from neurodegenerative disorders and, in the long run, to prevent these from occurring in the first place. Unfortunately, many scientists dealing with neurodegenerative diseases are too deeply invested in the current model to initiate change. The message needs to reach the public directly for real transformation. Pressure for reform must come from both inside and outside medicine.
References
Vaccaro, A., Dor, Y. K.., & Rogulja, D. et al., (2020). Sleep loss can cause death through accumulation of reactive oxygen species in the gut. Cell, 181(6), 1307-1328.
Nguyen, T. T., Zhang, X... & Jeste, D. V.et al., (2021). Association of loneliness and wisdom with gut microbial diversity and composition: an exploratory study. Frontiers in psychiatry, 395.
Navigating the Path Forward for Dementia in Canada: The Landmark Study Report #1
https://alzheimer.ca/en/research/reports-dementia/landmark-study-report…
Lam, V., Takechi, R., Hackett, M. J., Francis, R., Bynevelt, M., Celliers, L. M., ... & Mamo, J. C. (2021). Synthesis of human amyloid restricted to liver results in an Alzheimer disease–like neurodegenerative phenotype. PLoS Biology, 19(9), e3001358.
Nguyen, T. T., Zhang, X., Wu, T. C., Liu, J., Le, C., Tu, X. M., ... & Jeste, D. V. (2021). Association of loneliness and wisdom with gut microbial diversity and composition: an exploratory study. Frontiers in psychiatry, 395.
The buildup of neurofibrillary tangles of tau protein inside neurons in Alzheimer’s, Parkinson’s and other brain diseases which has been assumed was the culprit actually occurs in all aging cells, not just brain cells.
https://stanfordhealthcare.org/medical-conditions/brain-and-nerves/deme…




