Post-Traumatic Stress Disorder
The First Medical Tool to Robustly Predict PTSD
Persistent, elegant research yields a PTSD-prediction model clinicians can use.
Posted January 27, 2019
Trauma is a fact of life. It does not, however, have to be a life sentence. — Peter A. Levine
Patients, clinicians and healthcare systems — hospital leaders, researchers, and so on — need to be able to predict who is most likely to develop PTSD following a traumatic event. So far, this has been an elusive goal, though much research over the past few decades have produced fundamental data required to build good predictive models. If we know within a relatively short period of time who is most likely to get PTSD after a highly distressing experience, we can make informed decisions so that people needing interventions will receive them and people who don't do not. It would also improve the efficiency of how scarce resources are allocated, freeing them up to be used where they are needed.
Because psychiatry is still young from the point of view of understanding what is going on, because the brain and nervous system are so complicated and are indistinguishable from the body on an integrative level, psychiatry has fewer of the well-developed statistical tools, diagnostic and algorithmic, which general medicine and specialties often employ. Fields such as oncology and intensive care, for example, really track big data in order to make more effective medical decisions. No statistical approach can yet replace clinical judgment, and unless and until there is absolute certainty regarding outcomes, the moral and ethical dimensions of medical care remain essential.
Developing a robust model to predict PTSD in acute care settings
In order to enhance care for people exposed to traumatic circumstances, the aptly-named International Consortium to Predict PTSD (ICPP) was founded by an international, multicenter group of clinician-researchers. I met Dr. Arieh Shalev, one of the leading PTSD experts in the world and an important member of the ICPP who is affiliated with NYU Langone Medical Center, while responding to the WTC attacks of September 11th, 2001 at the sadly no longer extant St. Vincent’s Hospital in NYC. St. Vincent's was a beloved neighborhood and city hospital, right in the path of crowds fleeing Ground Zero, and a center of immediate response. For years until it was demolished, there was a touching and highly personal memorial on Seventh Avenue (part of installations at the 9/11 Memorial and Museum). Having a predictive tool then would have saved untold suffering now. The need for these tools in mental health cannot be overstated.
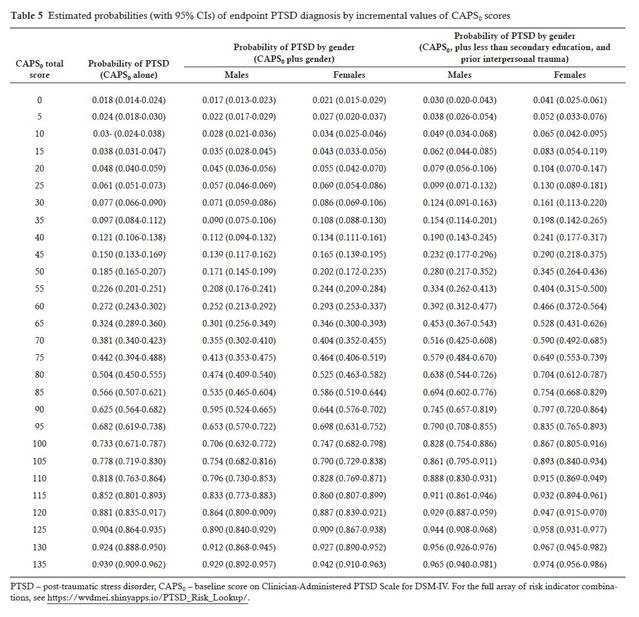
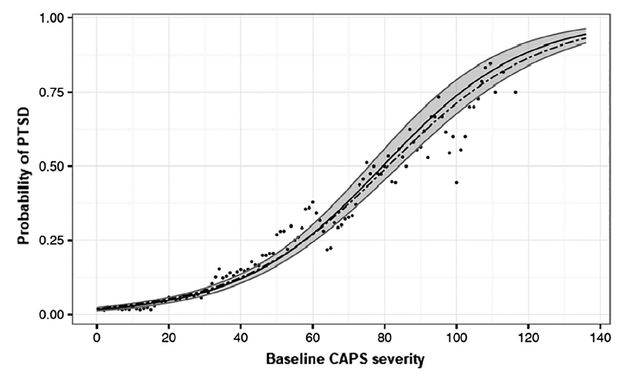
Prior research has developed useful scales to estimate PTSD symptom burden for clinical management, to identify treatment focus areas, and for diagnostic purpose. It is hard to use these tools to predict PTSD in the future because there isn’t a simple cut-off score, above which you get PTSD and below which you do not. Tools have to be probabilistic, like a growth chart—there is a curve, with the measure on the bottom and the probability along the side. You cross-reference the score on the chart, for a given patient, and it tells you the chance they’ll have PTSD. You can have a different chart for different risk groups, or use a table of numbers to cover more variables than a curve.
For PTSD with ICPP, this would mean using the Clinician Administered PTSD Scale for DSM-IV (CAPS) in a clinical or related setting (a Family Assistance Center, or a field hospital in the Sudan) in order to triage people to appropriate care — immediate intervention (psychological preventive treatment for trauma), lighter interventions, close tracking to follow for the emergence of worsening PTSD, follow-up for less affected people and long-term monitoring. Of note, the CAPS is based on DSM-IV criteria, and future work will update clinical tools to include a more inclusive definition of PTSD which includes mood-related and dissociative symptoms. The goal of having a useful and useable clinical tool achieved in the present work, however, is a huge victory, the result of years of hard work, much heart, and a ridiculous amount of collaboration.
The game-changing Estimating the risk of PTSD in recent trauma survivors: results of the International Consortium to Predict PTSD (ICPP) is published in the journal World Psychiatry (free access to the full article here; Shalev et al., 2019). The ins-and-outs of the statistical analysis are complicated, designed to ensure that the predictive model has been held to the same standards applied in other fields.
For example, the authors tested multiple predictive models with and without different methods to model the data, with and without risk factors included (e.g. female gender, lower educational level, and prior exposure to interpersonal trauma, from established previous research), and so on. They tested to make sure, because they were using pooled data from 10 studies, that differences among the studies did not distort the predictive model. They filled in cracks in the model with a nice form of statistical spackle called “Multiple Imputation using Chained Equations (MICE). They made sure that missing diagnostic information, such as the required four-week duration for symptoms to persist to meet the formal definition, didn’t affect the predictive power of the model. They tested different models for fit, and chose the best model.
There were 10 studies from a variety of national and cultural contexts (Asia, Australia, USA, Europe, South Africa), and 2,473 patients across the 10 studies who had been seen in 13 acute-care settings (e.g. emergency departments). To be included, patients had to have been assessed in the first 60 days, then had one or more follow-ups between 4 to 15 months following the initial trauma. Participants were on average 39 years old and were 37 percent women; 69 percent had been in a motor vehicle accident, 25 percent experienced non-interpersonal trauma, and 6 percent experienced interpersonal trauma. At the time of the final measure, 11.8 percent met diagnostic criteria for PTSD, which was nearly twice as high in women than men (16.4 vs. 9.2 percent) and significantly higher for interpersonal trauma than MVA or other traumas (27 percent vs. 5 and 13 percent).
Risk factors were confirmed on logistic regression, with higher rates of PTSD among: women, those with less than a secondary education, and prior interpersonal trauma. This is important to the final clinical application as, for instance, the baseline PTSD risk by CAPS score would be on a different curve for a woman with no other risks than a woman with lower education and prior interpersonal trauma. In practice, this might look like a basic app where you enter the relevant data, e.g. CAPS score and the presence or absence of risk factors, and it would report the PTSD risk and offer clinical recommendations.
How can this research be clinically used?
This data-driven advice could be included in clinical decision-making, and tailored to the particular person and their circumstances. Having this kind of risk estimate also helps to apply for required services in areas where health insurance requires prior authorization. Tracking outcomes to see if using this model leads to better long-term outcomes is important. It seems likely that making better choices about early intervention will lead to better outcomes, but following up to confirm and refine the model is critical.
Desirable refinements include the ability to estimate the time to onset of PTSD, the severity of future PTSD, which interventions work best under what circumstances, how much this data, how this model works with complex PTSD (cPTSD), and to see whether including additional PTSD and dissociative symptoms from more recent diagnostic criteria (e.g. DSM 5, ICD-10) significantly improves not only the predictive power, but importantly clinical decision making, monitoring, and outcomes.
Table of PTSD risk by CAPS score and risk factors: