Depression
Four Different Biotypes of Depression
Neuroscience research advances diagnosis and treatment.
Posted June 30, 2017
The impact of depression
Approximately 20 million Americans suffer from depression, and less than half of them are receiving specialized care. According to the CDC, as of 2012, 7.6 percent of Americans over the age of 12 had significant depression, which was higher among women, and worse in people 40 to 59 years of age. Only 35 percent of people reporting severe depression had met with a mental health professional within the last year. Over 40 percent with less severe depression reported that it had caused serious difficulty with function; the number was almost 90 percent for those with severe depression.
Over 40,000 Americans die by suicide yearly. In 2010 in the U.S. alone, depression was estimated to have cost $210 billion due to lost productivity and clinical costs. Globally, according to the WHO, 300 million people have depression, and close to 800,000 people die yearly from suicide, which is the second leading cause of death in people aged 15-29.
Standard treatments such as SSRI antidepressants are only fully effective for about 30 percent of patients but are partially effective for another 30 percent (STAR-D Trial). As a result, it often takes multiple medication trials in combination with other therapeutic approaches such as talk therapy to achieve even a modest response, let alone a full remission of symptoms and a full return to function.
The need for improved psychiatric care
Conventionally, as with the majority of psychiatric conditions, there are no formal biomarkers available for diagnosis and treatment monitoring with depression. In other areas of medicine there are many conditions for which it is routine to order diagnostic tests, provide treatment, and monitor response. Hypothyroidism is a basic example—patients come with characteristic complaints, which may be due to thyroid problems but could be related to other conditions, a panel of blood tests is ordered, and the results are generally definitive. Treatment and monitoring is usually straightforward, and effective for most patients.
Depression, in contrast, is diagnosed based on clinical features, and subtypes are based on the presence of certain symptoms over others. Treatment response is tracked subjectively, by clinical evaluation, by functional state, and sometimes using validated rating scales. There is no biological diagnostic test available for depression, and treatment selection is primarily based on clinical judgment and consensus guidelines.
Only recently have psychiatrists had access to patient-specific data to guide clinical decision-making, such as from pharmacogenomic testing, which while advancing is still of limited value. It is very difficult to predict which treatment will help which patient, leading to a "trial-and-error" approach which can take months to work for the 1/3 of people who don't respond at all to initial treatment.
Having robust biological markers to diagnose and treat depression (and other psychiatric disorders), crucially is missing though progress is being made. Of course, there are many important factors aside from diagnosis and treatment selection, personal and psychosocial factors, the importance of wellness and resilience, and so much more for a well-lived life than I'm focusing on right now, and I don't mean to take away from the importance of viewing the person as a whole. Rather, I believe that having a deeper understanding of what is really going on in the brain will enrich the experience of being human, though as with any technological advances, caution is prudent.
The brain from a network theory perspective
The brain is a highly complex organ. It's elegant and beautiful, and key to who we are, and of course intimately a part of the body and not just a brain in a vat. Understanding how the brain works requires more sophisticated models which have only recently become available. Until the last couple of decades or so (with some exceptions), basic approaches to neuroscience were reductionistic—based on breaking things down into easier to understand parts. Part of this is because although we could conceptualize the brain as a system, the mathematical and computational tools have only been available recently. It's important to recognize this shift to a complex model of the brain, because it is a game changer both conceptually and in terms of being able to design more powerful tools based on a more accurate understanding of how the brain actually works.
So psychiatry has tended to focus on simpler models like correcting a "chemical imbalance"—serotonin levels are low, so we'll give a medicine which increases serotonin. This is really just a metaphor, and not an accurate one. There are many different families of serotonin receptors all over the brain, and they are on the surface of neurons and other cells around the body. When we prescribe a medication based on serotonin function, we don't really understand what it is doing, both on the big picture level and on a microscopic level, how such a medication causes changes with the cells, and moreover how these changes lead to therapeutic benefits or adverse reactions—and whether a given medication will or won't work for a given person.
Similarly, research has looked at what different areas of the brain do, correlating illnesses with higher or lower activity in various brain regions. More sophisticated but still reductionistic, we look at different "circuits" in the brain, how key areas are wired together and how this relates to healthy function and problematic dysfunction. Sometimes this approach works pretty well—when a brain region is a key hub for specific functions or a specific circuit is closely tied to pathology—but it is more accurate and powerful to see the brain as a system, in which different parts are interconnected to give rise to the overall function of the brain, the mind.
The systemic perspective is powerful. From this point of view, the unit of understanding, and the target of therapeutics, are brain networks. Different brain regions, much like the different nodes on the Internet that dynamically form the World Wide Web, are interconnected in complex ways in various structural and functional networks. They provide stability over time along with the ability to rapidly adapt to changing conditions, and when functioning smoothly maintain flowing balance to provide resilience in the face of environmental changes.
Until recently, it was too difficult to get a deep understanding of brain networks because the mathematics involved were not as well developed, the application to neuroscience was not as fleshed-out, and importantly because the required computing power wasn't there yet. Recently, due to advances in mathematics and computer technology, we can now start to see the big picture. Because so much technical knowledge is involved, it is hard to grasp. This widens the gap between researchers and almost everyone else—practicing clinicians, patients, and the lay public. Therefore, I use some technical terms while trying to avoid unnecessary jargon.
Groundbreaking research
A major advance in the network understanding of depression was published recently in the prestigious journal Nature Medicine by a high-powered group of researchers. In their paper, the authors describe the findings of their elegant work, the purpose of which was to analyze brain scans from more than 700 subjects, comparing the resting activity of depressed patients' brains with non-depressed patients' to determine significant differences in patterns of brain activity.
Their approach was to analyze the data for patterns that could be biomarkers for depression, identifying different networks representing different subtypes of depression. Rather than the conventional approach—defining different types of depression based on clinical features—their approach is designed to map out differences in networks based on actual brain activity to develop consistent biomarkers to diagnose depression. They used complicated methodologies ("canonical correlation analysis" and "hierarchical clustering") as well as artificial intelligence (or "machine learning") to measure connectivity and map out networks associated with depression.
Ultimately, this information could be used to guide treatment selection by identifying which subtypes respond to which treatments. In principle, it should then be possible to use neuroimaging to identify which type of depression a patient has, and to guide treatment planning.
Major findings
They found that there are four subtypes of depression, called "biotypes," illustrated below. They are color coded to show which brain areas have the most connectivity within each biotype. If readers are interested in learning more about the specific anatomic areas, you may find this 3D brain tool a useful reference.
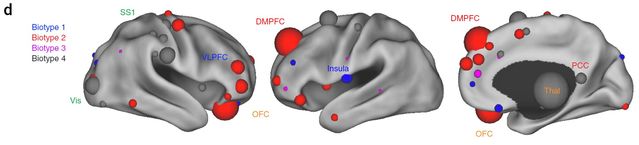
Researchers identified two major groups of network patterns characterizing depression involving 1) frontostriatal and orbitofrontal areas or 2) the limbic system, including areas such as the amygdala, ventral hippocampus, ventral striatum, subgenual cingulate and lateral prefrontal cortex.
The first group correlates with symptoms of anhedonia (difficulty experiencing pleasure) and psychomotor retardation (difficulty initiating movement and sluggish movement) and the second group with anxiety and insomnia. They used a clinical rating tool called the "HAM-D" (Hamilton Depression Rating Scale) to match network analysis with symptoms. In a basic but incomplete sense, the first group broadly has to do with top-down control, and the second group with emotional regulation on a deep brain level.
They found that all biotypes share certain core clinical features—low mood, anhedonia, fatigue and lack of energy—associated with anatomic areas such as the insula, orbitofrontal cortex, ventromedial prefrontal cortex, ventromedial prefrontal cortex, and multiple subcortical regions.
The four biotypes vary depending on which brain regions were connected with and distinct from one another, representing 23.6 percent, 22.7 percent, 20 percent and 33.6 percent of the sample. They correlate with different patterns of connectivity, and moreover with specific and distinct sets of clinical symptoms.
Here is a breakdown of which clinical symptoms go with which biotype:
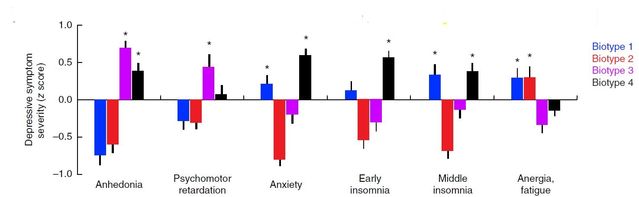
The clinical picture, with some overlap, is distinct for each biotype. Types 1 and 4 have increased anxiety related to fear-based regions; types 3 and 4 show more anhedonia and psychomotor retardation related to areas governing reward, control of movement, and initiating actions; and types 1 and 2 have lower energy and fatigue, related to brain areas involved with motivation and decision-making. Regardless of biotype, the overall severity of depression was comparable among the 4 groups, though slightly less severe for type 2. Importantly, the biotypes do not correlate well with existing clinical subtypes of depression.
Implications for diagnosis and treatment
They found that using machine-learning, they were able to correctly identify biotypes of depression and distinguish them from a non-depressed subjects, similar to a diagnostic test like an MRI for a brain injury. This initial application is a possible precursor to a diagnostic tool which could be used in regular clinical practice. They also found that the biotypes, unlike clinical subtypes, tend to remain consistent over time, suggesting that in some respects, biotypes may be a more reliable tool than doctor or patient assessments.
Notably, they were able to identify which biotype responded better to transcranial magnetic stimulation (TMS), a targeted treatment for depression which is often used to activate areas of the left frontal lobe of the brain. TMS was most effective in biotype 1, followed by biotype 3, but was not very effective for biotypes 2 and 4. As a TMS provider, this is of particular interest to me. A similar approach could be used to work out what other treatments work best for different biotypes of depression, allowing for more sophisticated personalized care.
Future directions
Because ineffective treatments are costly and time-consuming, disappointing, delay definitive treatment, and may lead to a worsening of depression and negative outcomes, having a way to tell what will work best would be an essential clinical tool. It will be useful for research to identify which therapies or combination of therapies (medications, talk therapies, and other approaches) will work best for which type of depression, and perhaps even to design personalized treatments which will work well for specific people based on biomarkers.
We can imagine a time in the not-so-distant future when a patient comes to the office for psychiatric evaluation, and we order diagnostic tests—functional brain imaging, genetic testing, perhaps a blood test for biological response to medication treatment if appropriate, and maybe even a computer simulation of how different treatment options would work, if administered, or even a treatment designed for that person, as is already possible with some cancer treatments.
In addition to clinical judgment and patient-specific factors, we would provide a comprehensive, tailored treatment plan which could include different therapeutic approaches. Early on, we could check to see if treatment is working, again using biomarkers which would be earlier indicators than clinical observations, and get information to guide changes to the treatment plan, if necessary. This sounds expensive, but would pay for itself in quality of life and savings down the road from reduced direct and indirect costs of treatment-resistant depression.
Depression is a difficult-to-treat condition which causes great suffering and costs individuals, families and society more than statistics can convey. Achieving a deeper understanding and taking a step toward refined diagnosis and treatment using empirically-based biomarkers is a major advance, and the first chapter in a developing story.
Please send questions, topics or themes you'd like me to try and address in future blogs, via my PT bio page.
References
Drysdale AT, Grosenick L, Downar J, Dunlop K, Mansouri F, Meng Y, Fetcho RN, Zebley B, Oathes DF, Etkin A, Shatzberg AF, Sudheimer K, Keller J, Mayberg HS, Gunning FM, Alexopoulos GS, Fox MD, Pascual-Leone A, Voss HU, Casey BJ, Dubin MJ & Liston C. (2016). Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nature Medicine, vol. 23, no. 1, January.




