Psychiatry
A Roadmap to the Future of Psychiatry
...and it's not the DSM-5
Posted June 1, 2017 Reviewed by Hara Estroff Marano
The modern era of psychiatry began with some European doctors who carefully catalogued symptoms of the then mostly untreatable illnesses in the severely ill population of large psychiatric hospitals. Doctors such as Kraepelin noted differences between disorders based on mood (such as major depression and bipolar disorder) and those which had a psychotic degeneration as the central feature (schizophrenia, which Kraepelin called ‘dementia praecox.’) By the early part of the 20th century, enormous psychiatric hospitals housed thousands upon thousands of people.
In America, interest in cataloging and defining different mental illness came first from the Army, which made a manual to describe symptoms of people unfit to serve due to mental illness. That manual became the basis for the first “Diagnostic and Statistical Manual,” or laundry list of symptoms and diagnoses based mostly on observation and need to catalogue and track such illnesses.
By the time the DSM II came around in 1968, psychoanalysis and the ideas of Freud had hugely influenced American psychiatry, and wildly speculative causes of disorders (such as the “schizophrenigenic mother”) made the slender document half a description of symptoms, half (now mostly discredited) psychoanalytic theory. While modern therapists may scoff at these theories, it was a bold attempt by doctors at the time who had no way to peek into the brain as it worked to figure out why bizarre and seemingly unexplainable symptoms such as wild mood swings, sociopathy mania, and psychosis might occur.
By 1968, however, treatments such the early antipsychotics, lithium, insulin shock and electroshock therapy were found to often improve severe depression, psychosis, and mania. These biologic treatments belied some psychoanalytic theory…we know now it does little good to spend five hours a week with a schizophrenic patient on the couch free-associating, and as medications and biologic treatments evolved, so have therapies for all diagnoses, focusing more on support, coping skills and solutions and less on the unconscious.
In 1980, the DSM III came out, and for many psychiatric disorders, the prevailing theory was that biology plus environment led to common sets of psychiatric symptoms. Psychiatrists knew by then that the there was something biologic going on in the brain to cause these symptoms, but also knew they didn’t have the scientific tools to figure out the pathology itself. Therefore they made the DSM III to be deliberately atheoretical: It is just a boring recipe list of typical symptoms and combinations of symptoms meant to help with research, in the hope that future doctors would use modern tools to add pathologic and biologic explanations to the major disorders. Psychiatrists also knew that it was likely several different disorders that mostly looked alike were combined into one big basket, schizophrenia being a good example (with paranoid types, disorganized types, etc.).
Since 1980, the DSM-IV and DSM-5 have been published in succession, all similar, ever-growing recipe lists of symptoms. They are necessary for research and also for medical billing, but they are the equivalent of calling a runny nose, cough, and fatigue a "cold" when such symptoms could actually be caused by viruses, bacteria, or even combinations of allergies or superinfection on cancer or…the lists of actual possible pathologies goes on and on.
Psychiatry has been the equivalent of being an infectious disease doctor without a microscope or ability to culture the actual cause of the problem and then treat accordingly. We see the symptoms and we use our skills and experience to make the best educated guess as to what is going on, try to rule out a few medical causes, and go from there with therapy and/or medications. A lot of it, even after all these years, remains a guessing game.
However, the combination of some recent basic science innovations has finally given psychiatry windows to pathology in the living brain. MRIs, PET scans, functional MRI, and SPECT scans tell us more about small and large changes in structure, function, and metabolism of the brain. Large-scale genetic testing has narrowed down some common genes in people with psychiatric illnesses.
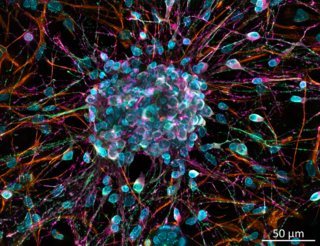
The ability to de-differentiate skin cells into a precursor cell, and then make that cell into an active neuron means we can track what effect genetic changes have on the function of receptors and ion channels in the neurons of living humans with no psychiatric disorders versus those with bipolar disorder, for example. We’ve been able to develop animal models of many of these pathologies and track treatments for specific genetic changes in humans.
It’s just the beginning. But in the near future, we may be able to ditch the DSM-5 altogether. In lieu of: Here is a man with major depressive disorder and borderline personality traits, we can say: Here is someone with increased ability to breakdown neurotransmitters plus decreased ability to use those neurotransmitters he has left due to genetic issues with making active forms of vitamins, overlaid on a history of trauma or dramatic and damaging relationships. We can design studies and then therapies based on actual pathology rather than guessing games…replace neurotransmitters, improve membrane signaling or reduce pathologic excitotoxicity based on the known genetic profile and a combination of exercise, medications, nutritional supplements, improved sleep, and psychotherapies.
The next article will have more details about the actual known genes, related pathologies, and the state of the evidence and how it might guide treatments even today. It’s an exciting time to be a psychiatrist.
Copyright Emily Deans MD




