Eating Disorders
What to Do When Eating Disorders and Obesity Coexist
An interacting and complex relationship.
Posted November 2, 2022 Reviewed by Gary Drevitch
Key points
- Obesity is the medical condition most frequently observed in people with eating disorders.
- Eating disorders and obesity, when they coexist, tend to interact negatively with each other and make treatment more problematic.
- Weight loss is always contraindicated when obesity coexists with bulimia nervosa.
- Weight loss is not contraindicated when obesity coexists with binge-eating disorder, but with the current treatments, it is often unsatisfactory.
Obesity is the medical condition most frequently observed in people with eating disorders. It often coexists with binge-eating disorder and with some cases of bulimia nervosa. Obesity can precede the onset of the eating disorders, sometimes representing a risk factor for its onset, or may be partly the consequence of recurrent binge-eating episodes. Eating disorders and obesity, when they coexist, tend to interact negatively with each other and make treatment more problematic.
Prevalence
Among seeking-treatment patients for obesity, about 9-10% meet the diagnostic criteria for binge-eating disorder. However, in the same population, binge-eating episodes have been reported in about 30% of cases. There is no reliable data on the prevalence of bulimia nervosa in obesity, but the coexistence of the two conditions does not seem to be very frequent.
Risk Factors
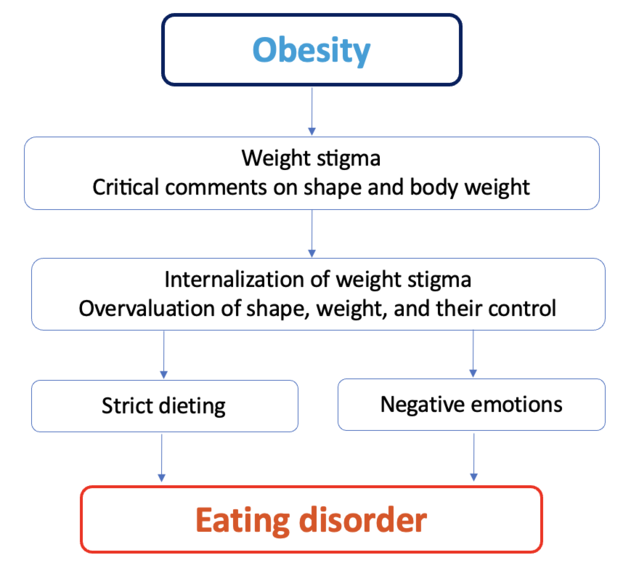
Studies have revealed that pre-morbid obesity is a potential risk factor for bulimia nervosa, binge-eating disorder, and atypical anorexia nervosa. It has been hypothesized that the weight stigma of Western countries puts people with obesity at increased risk of receiving critical comments about their shape and weight and discrimination from others. These negative experiences increase the probability of internalizing the “thin ideal” and developing the overvaluation of shape and weight (i.e., judging themselves predominantly or even exclusively in terms of shape, weight, and their control). The latter is considered the core psychopathology of most eating disorders and promotes the adoption of rigid and extreme dietary rules, often implicated in the onset and maintenance of binge-eating episodes (see Figure 1).
Interactions Between Eating Disorders and Obesity
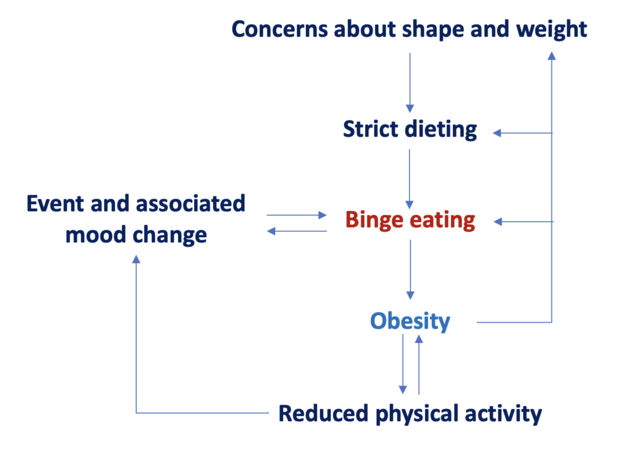
When they coexist, eating disorders and obesity interact negatively with each other through three main mechanisms (Figure 2):
- Binge-eating episodes promote weight gain.
- Excess weight increases concerns about body shape and weight and encourages the adoption of a strict diet and other extreme weight control behaviors, which, in turn, increases the risk of binge-eating episodes.
- Excess weight is often associated with reduced physical activity levels and an increased risk of having negative emotional states that can trigger binge-eating episodes.
Clinical Consequences
When obesity coexists with binge-eating disorder, it is characterized by worsening medical comorbidities and physical disability.
Available data indicate that individuals with binge-eating disorder have a greater frequency of metabolic syndrome components (i.e., dyslipidemia, hypertension, and type 2 diabetes) and cardiometabolic risk than those with no history of an eating disorder.
It has been hypothesized that in people with binge-eating disorder, increased weight-independent medical comorbidities are likely to be the result of their unhealthy lifestyle, characterized by smoking, low levels of exercise, alcohol abuse, and poor eating, with recurring binge-eating episodes involving eating foods high in fat, sugar and/or salt, but lacking in vitamins and minerals. This may explain why people with binge-eating disorder and obesity often suffer from both the typical complications associated with obesity (e.g., metabolic syndrome and type 2 diabetes) and other weight-independent medical problems such as irritable bowel syndrome, as well as complications related to alcohol abuse and smoking; neck, shoulder, and lower back pain; and chronic muscle pain.
Is Weight Loss Indicated?
Weight loss is always contraindicated when obesity coexists with bulimia nervosa. Indeed, binge-eating episodes are largely maintained by the attempt to adhere to extreme and rigid eating rules and/or severe dietary restriction (i.e., undereating in physiological terms). People with bulimia nervosa tend to react negatively, often dichotomous, to the almost inevitable breaking of the dietary rules adopted to lose weight. Even a small transgression tends to be interpreted as evidence of a lack of self-control and results in temporary abandonment of the effort to restrict the diet, resulting in a binge-eating episode. This, in turn, maintains the overvaluation of shape and weight by intensifying concerns about being unable to control shape, weight, and eating and encourages further dietary restriction, thus increasing the risk of other binge-eating episodes. With this in mind, moderate weight loss should only be considered in patients with obesity and bulimia nervosa after a prolonged period of remission from the eating disorder—at least one year.
When obesity coexists with binge-eating disorder, there is no absolute contraindication to weight loss. However, while the available treatments (e.g., cognitive behavior therapy [CBT] for eating disorders, interpersonal psychotherapy, CBT-based guided self-help, and pharmacological agents) are effective in reducing the frequency of binge-eating episodes, their impact on long-term weight loss in patients with episodes of binge-eating is poor.
To find a therapist, visit the Psychology Today Therapy Directory.
References
Dalle Grave, R., & Calugi, S. (2020). Cognitive behavior therapy for adolescents with eating disorders. New York: Guilford Press.
Dalle Grave, R., Sartirana, M., & Calugi, S. (2021). Complex cases and comorbidity in eating disorders. Assessment and management. Cham, Switzerland: Springer Nature.
Dalle Grave, R., Sartirana, M., El Ghoch, M., & Calugi, S. (2018). Treating obesity with personalized cognitive behavioral therapy. Cham: Springer.


