Eating Disorders
Gastrointestinal Symptoms, Dieting, and Eating Disorders
How to prevent the trigger or aggravation of feeding and eating disorders.
Posted October 3, 2022 Reviewed by Gary Drevitch
Key points
- Elimination diets are frequently used to manage gastrointestinal symptoms.
- Elimination diets may trigger or aggravate feeding and eating disorders in some people.
- Before adopting an elimination diet to manage gastrointestinal symptoms a feeding and eating disorder or a risk to develop it should be excluded.
Elimination diets are frequently used to manage gastrointestinal symptoms, such as abdominal pain, bloating, nausea, constipation, and diarrhea, which do not have an organic explanation.
The most common foods recommended to exclude are fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAPs). This is a category of carbohydrates found in wheat, beans, onions, garlic and other foods that tend to ferment in the intestine and retain water from the mucous membrane. Other common eliminated foods are eggs, soy, dairy, gluten, caffeine, fructose, food additives (e.g., food colorings and aspartame), histamines (e.g., found in fermented foods and beverages like wine, yogurt and sauerkraut), and sulfites (e.g., found in baked goods, soups, jams and canned vegetables).
Some studies have shown that the FODMAP diet, when used appropriately, can relieve the physical symptoms of irritable bowel syndrome in a subgroup of people. However, as I described in a previous post, recent studies have also reported that elimination diets may trigger or aggravate feeding and eating disorders in some people. For this reason, before adopting an elimination diet to manage gastrointestinal symptoms, a screening to exclude the presence of a feeding and eating disorder or characteristics associated with an increased risk of their development should always be done.
Features indicating the presence of a feeding and eating disorder in a person with gastrointestinal symptoms
The prevalence of functional gastrointestinal symptoms has been found in about 86 percent of patients with anorexia nervosa and 10-20 percent of adults with avoidant/restrictive food intake disorder (ARFID) symptoms. These data explain why the elimination of specific foods to manage gastrointestinal symptoms is a common behavior reported by people with feeding and eating disorders.
The presence of an eating disorder should be suspected when gastrointestinal symptoms, food avoidance, and restriction are associated with a fear of gaining weight or of becoming fat, overvaluation of shape and weight, and/or other extreme weight control behaviors (e.g., self-induced vomiting, misuse of laxatives and excessive exercising).
It is more complex to understand if one has an eating disorder when gastrointestinal symptoms, food avoidance/restriction, poor nutritional status, and quality of life impairment are not associated with the fear of weight gain and concerns about shape and weight. In these cases, the presence of an eating disorder should be suspected if one does not recognize the medical seriousness of their low weight and/or positively evaluates the restriction/avoidance of food. In addition, the overvaluation of food avoidance and restriction occurs not only because it helps mitigate gastrointestinal symptoms but also because it is used to feel in control and as a predominant domain of self-evaluation. These cases have been sometimes termed “non-fat phobic anorexia nervosa.”
The presence of ARFID should be suspected when there is a generalized avoidance of food in response to anxiety about potential gastrointestinal symptoms, even during periods of low symptom activity. In addition, people with ARFID often recognize the medical seriousness of their low weight.
The presence of an eating disorder or ARFID associated with gastrointestinal symptoms contraindicates the use of an elimination diet. In these cases, treating the feeding and eating disorder is a priority, and its remission is often associated with a marked improvement of gastrointestinal symptoms.
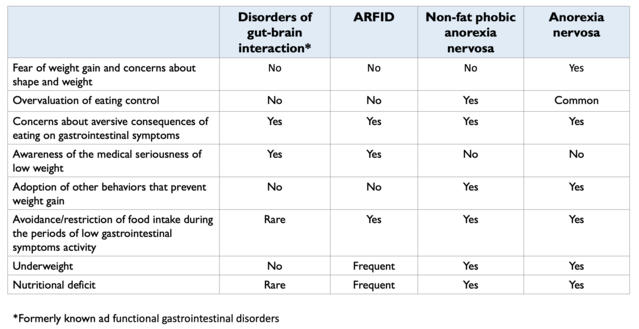
Table 1 describes the features that can help distinguish the presence of feeding and eating disorders in people with gastrointestinal symptoms who adopt an elimination diet.
Features indicating a person with gastrointestinal symptoms is at risk of developing a feeding and eating disorder
Understanding if one person with functional gastrointestinal symptoms is at risk of developing a feeding and eating disorder by adopting an elimination diet is not easy.
The characteristics to consider that could increase the risk of developing an eating disorder are female gender, adolescence, excess weight or low weight in childhood and early adolescence, having received negative comments about shape and weight, some personality traits (e.g., perfectionism, low self-esteem), and a family history of eating disorders.
ARFID, on the other hand, appears more likely to develop in women of normal weight when they lose more than 5 kg of weight, in those who report symptoms in the stomach or lower gastrointestinal tract, and when avoided and restricted foods are not only associated with gastrointestinal symptoms. However, the symptoms of ARFID in children are often observed in males and those who show little interest in food and/or avoid food for its sensory characteristics.
In people at risk of developing feeding and eating disorder, gastrointestinal symptoms should be managed with recommended treatments for gut-brain interaction disorders that do not involve the elimination of specific foods (e.g., cognitive behavioral therapy for irritable bowel syndrome or drugs to manage specific symptoms such as constipation, diarrhea, and abdominal pain).
Should I start an elimination diet if I have not or am not at risk of a feeding and eating disorder?
Even when a feeding and eating disorder or potential risk factors for its development have been ruled out, the pros and cons of adopting an elimination diet to manage gastrointestinal symptoms should always be carefully evaluated, as it may increase the risk of nutritional deficits and psychosocial problems.
If the medical advice is to adopt an elimination diet, it is advisable to be followed by a certified dietician expert in managing gastrointestinal diseases who can identify the early signs of a feeding and eating disorder or nutritional deficits and psychosocial problems.
As general advice, I suggest avoiding adopting an extreme and rigid elimination diet because a gradual and flexible approach to elimination diet therapy has been shown to improve gastrointestinal symptoms with a low risk of developing adverse nutritional and psychosocial effects.
References
Dalle Grave, R., & Calugi, S. (2020). Cognitive behavior therapy for adolescents with eating disorders. New York: Guilford Press.
Dalle Grave, R., Sartirana, M., & Calugi, S. (2021). Complex cases and comorbidity in eating disorders. Assessment and management. Cham, Switzerland: Springer Nature.




