Eating Disorders
How Emotions Affect Eating Disorders
When changes in eating are triggered by events and associated mood changes.
Posted June 2, 2022 Reviewed by Lybi Ma
Key points
- Events and emotions often influence eating behavior, and this association is also common in people with eating disorders.
- Some with eating disorders suffer mood intolerance and use dysfunctional mood modulation behaviors (self-harm, substance use)
- Events and emotions influencing eating may be addressed with proactive problem-solving and specific mood intolerance procedures.
Events and emotions often influence people's eating behavior, and this association is also common in people with eating disorders. The change in eating triggered by events and associated mood changes contribute to the maintenance of the eating disorder and tend to create an obstacle to change. For these reasons, events and emotions should be addressed by the treatment.
Common events that trigger negative emotions in people with eating disorders
The most common events likely to trigger negative emotions (for example, anxiety, fear, sadness, disgust, anger) in people with eating disorders are the following:
- Adverse shape or weight-related events (for example, weight changes, clothes feeling tighter, mirror checking, feeling fat, receiving critical comments from others)
- Adverse eating-related events (for example, eating an avoided food, eating too much binge eating, feeling full)
- Adverse events in general (for example, failure to perform well in a sports competition or at school, being rejected or told off, or other)
What are the changes in eating disorder features associated with events and emotions?
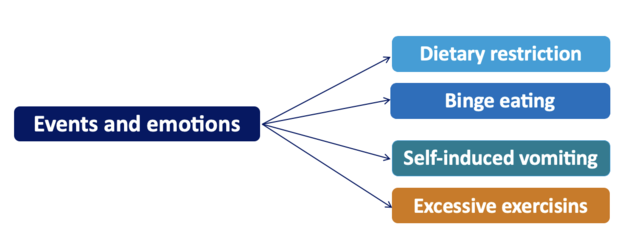
The specific dietary changes associated with events and related mood changes in people with eating disorders are eating in an uncontrolled way (binge eating) or eating less or fasting. However, in some people, the events and associated mood changes are associated with an intensification in exercising or the frequency of purging (see Figure 1).
What are the mechanisms responsible for this association?
The principal mechanisms responsible for the association between events, moods, and eating are the following:
- Binge-eating episodes can distract from adverse events and from problems that cause anxiety and mitigate intense and intolerable emotional states. The same effect on the modulation of mood can also be achieved via self-induced vomiting and or excessive exercising.
- Eating less can help people feel in control when events are perceived to be out of control.
- Overeating can be a way to achieve gratification.
- Eating less can be a way to influence the behavior of others, for example, as a manifestation of feelings such as anguish or anger. This behavior is typical of underweight adolescent patients, who, for example, may stop eating in response to an argument with their parents.
When to address events and moods?
Enhanced cognitive behavior therapy (CBT-E), an evidence-based treatment for all eating disorders, assesses whether events and moods contribute to the maintenance of the eating disorder after having helped the person adopt a regular eating pattern in the first stage of the treatment. If so, they need to be addressed directly and effectively. This mechanism is recognizable when there are repeated deviations from regular eating or planned meals and snacks, which can be traced back to external events or changes in mood. These deviations may manifest as recurrent binge-eating episodes, skipping meals and or snacks, and or repeated episodes of self-induced vomiting or excessive exercising.
How are addressed events and emotions influencing eating?
CBT-E helps people with eating disorders to address events and associated mood changes influencing eating using two main strategies:
- Proactive problem solving: used in any case.
- Mood intolerance procedures: used in a subgroup of cases.
However, improvement in mood is also seen in the context of the CBT-E because of the following changes:
- Regular eating.
- Reduction in dietary restriction.
- Normalization of body weight.
The proactive problem-solving procedure
Essentially, the persons are asked to look ahead, at the beginning of the day and every time they eat, to the remainder of the day and try to predict when a problem might arise. When they foresee a potential problem, they should practice problem-solving there and then (in writing) and then act on the solution identified. The following day, patients should review their problem-solving attempts and write the outcome of their using the procedure on the back of their monitoring record. Their therapist will go over their experience with them in the next session.
Mood intolerance procedures
Mood intolerance may co-exist with an eating disorder and, when it does, tends to maintain it. Mood intolerance has two principal components:
- Extreme sensitivity to intense (mainly aversive) mood states. This is characterized by an inability to accept and deal appropriately with them.
- The use of dysfunctional mood-modulation behaviors to reduce awareness of an intense mood state and neutralize it.
Dysfunctional mood-modulation behaviors may take on two forms:
- Self-harming (for example, cutting or burning the skin).
- Taking a psychoactive substance (for example, alcohol or other substances).
People with both an eating disorder and mood intolerance often discover that some behaviors characteristic of eating disorders (for example, binge eating, self-induced vomiting, and excessive exercising) can be used to cope with their negative emotions and make them feel better in the short term (see Figure 2).
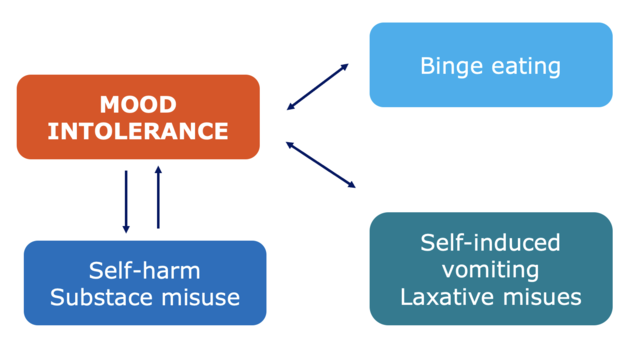
However, such behaviours may also serve to maintain the eating disorder. To successfully treat the eating disorder, mood intolerance needs to be tackled directly by means of an approach that overlaps with elements of dialectical behavior therapy (DBT) (Linehan, 1993) integrated with the procedures of CBT-E used to address the eating disorder maintaining mechanisms.
For more details see the CBT-E mood intolerance module described in the CBT-E guides (Fairburn 2008; Dalle Grave & Calugi, 2020).
References
Dalle Grave R, Calugi S. Cognitive behavior therapy for adolescents with eating disorders. New York: Guilford Press; 2020.
Fairburn CG. Cognitive behavior therapy and eating disorders. New York: Guilford Press; 2008.
Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993.




