Health
Opening Mental Health Notes: 7 Tips to Prepare Clinicians
New federal laws mandate sharing clinical notes; how to benefit from this change
Posted October 19, 2020 Reviewed by Lybi Ma
This blog post was co-authored with Charlotte Blease, Ph.D., Keane Scholar at OpenNotes, Beth Israel Deaconess Medical Center/Harvard Medical School.
In the United States, November 2nd, 2020 marks an important turning point in medicine. New federal rules will be implemented mandating – with few exceptions – that healthcare providers must offer patients online access to their clinical notes (“open notes”). Access will not just be to lists of medications, appointment dates, and test results but to the very words written by clinicians. Some clinicians may be nervous or unsure how best to share notes; and in this post, we outline what the new law is, what open notes is, and seven tips that will make the process of sharing notes both easy and clinically beneficial for both you and the patient.
Already more than 52 million Americans have access to their notes via online health portals. Surveys show patients’ experiences with reading their notes are overwhelmingly positive, and patients reporting doing a better job taking their medications as one of several benefits. But a small number of patients do report being more confused or worried about what they read in their notes. Several small-scale studies in psychiatric settings are also promising, though more research is needed to explore the experiences of persons with serious mental illness. While clinicians often worry that sharing notes with patients will lead to complaints, confusion, or rupture of the alliance with patients – evidence for such is scarce. One healthcare system, the Veterans Health Administration, has had years of experience sharing notes – including in-patient psychiatry notes: we aware of no cases of patient harm of legal issues at the VHA.
What will the federal ruling mean for mental health clinicians? Psychotherapy notes will be excluded in the new ruling. And the rules permit “information blocking” if doing so “…will substantially reduce the risk of harm[D(-M1] ” to a patient or to another person. Licensed health professionals can decide what constitutes a substantial risk when working “…in the context of a current or prior clinician-patient relationship”. Lacking clear evidence in mental health contexts, this leaves considerable scope for interpretation. On the other hand, under the rules, the burden will be on clinicians to justify denying patient access. Complicating matters further, in communications from the Office of the National Coordinator for Health Information Technology, we are hearing that psychological distress does not meet the definition of harm in the rules.[CB2]
In adhering to the new rules, mental health clinicians must balance transparency and respect for patient autonomy, while preserving the necessary clinical detail in notes. Drawing on existing research, we recommend the following seven hints and tips to prepare patients and for writing mental health notes:
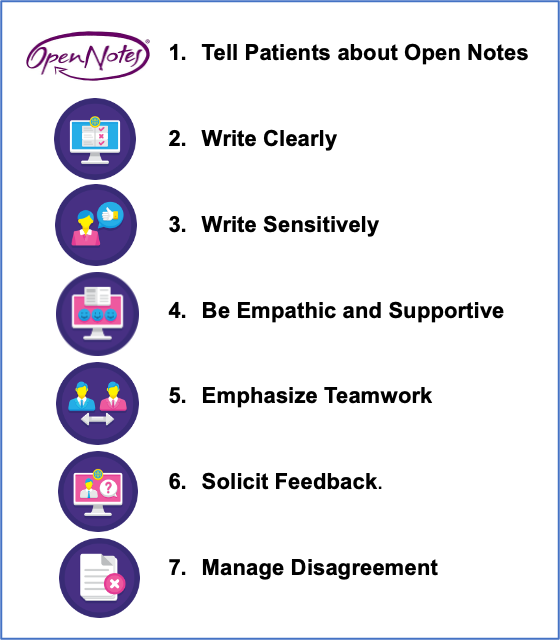
1. Tell patients about open notes: Inform patients about the practice, including the purpose of medical notes. Advise them there are benefits of reading their notes in helping to remember their care plan, appointments, and the rationale for treatments. Inform them there is a small risk they may be upset by what they read, but that ongoing support and clarifications can be discussed during visits.
2. Write clearly. Avoid too much medical jargon and acronyms but don’t lose the detail. Write as if both the patient and another clinician are in the room, looking over your shoulder.
3. Write sensitively. Some conventional wording may be perceived as offensive: e.g., “patient denies” or “patient refused”. Adopt phrasing such as “The patient stated that they do not use recreational drugs” or “The patient chose not to pursue treatment”. Be mindful of potentially offensive acronyms such as f/u (“follow up”) or SOB (“shortness of breath”). If you use a certain diagnosis in your note, be sure the patient is aware of it and what it means.
4. Be empathic and supportive: Write not just about the patient’s pathology, but about their progress.
5. Emphasize teamwork: Describe the treatment plan and goals. Include brief statements that speak directly to the patient: e.g., “I see us working together as a team”.
6. Solicit feedback: Surveys show that many patients do spot errors or omissions in their notes, helping to close the feedback loop on care. Encourage feedback and advise that any issues can be resolved during visits.
7. Manage disagreement: Disagreement may arise but use patient quotations to document the tension: e.g., “Although you differ on the diagnosis, and I cannot change my medical judgment, I will record your disagreement”. Such occasions may also be presented as opportunities for more open dialogue, and deeper discussion.
Open notes may be new to many mental health clinicians, and change is never simple. While sharing notes with patients may create apprehension, following these simple tips can make the experience beneficial for all parties.
References
https://www.hhs.gov/sites/default/files/privacysummary.pdf
Walker J, Leveille S, Bell S, Chimowitz H, Dong Z, Elmore JG, Fernandez L, Fossa A, Gerard M, Fitzgerald P, Harcourt K. OpenNotes after 7 years: patient experiences with ongoing access to their clinicians’ outpatient visit notes. Journal of medical Internet research. 2019;21(5):e13876.
DesRoches CM, Bell SK, Dong Z, Elmore J, Fernandez L, Fitzgerald P, Liao JM, Payne TH, Delbanco T, Walker J. Patients managing medications and reading their visit notes: a survey of OpenNotes participants. Annals of internal medicine. 2019 Jul 2;171(1):69-71.
DesRoches CM, Bell SK, Dong Z, Elmore J, Fernandez L, Fitzgerald P, Liao JM, Payne TH, Delbanco T, Walker J. Patients managing medications and reading their visit notes: a survey of OpenNotes participants. Annals of internal medicine. 2019 Jul 2;171(1):69-71.
Peck P, Torous J, Shanahan M, Fossa A, Greenberg W. Patient access to electronic psychiatric records: a pilot study. Health policy and technology. 2017 Sep 1;6(3):309-15.
Kipping S, Stuckey MI, Hernandez A, Nguyen T, Riahi S. A web-based patient portal for mental health care: benefits evaluation. Journal of medical Internet research. 2016;18(11):e294.
Blease C, O'Neill S, Walker J, Hagglund M, Torous J. Sharing notes with mental health patients: balancing risks with respect. Lancet Psychiatry. 2020, Feb. S2215-0366(20)30032-8. Online ahead of print
Dobscha SK, Kenyon EA, Pisciotta MK, Niederhausen M, Woods S, Denneson LM. Impacts of a web-based course on mental health clinicians’ attitudes and communication behaviors related to use of OpenNotes. Psychiatric Services. 2019 Jun 1;70(6):474-9.
Klein JW, Jackson SL, Bell SK, Anselmo MK, Walker J, Delbanco T, Elmore JG. Your patient is now reading your note: opportunities, problems, and prospects. The American journal of medicine. 2016 Oct 1;129(10):1018-21.
Bell SK, Delbanco T, Elmore JG, Fitzgerald PS, Fossa A, Harcourt K, Leveille SG, Payne TH, Stametz RA, Walker J, DesRoches CM. Frequency and Types of Patient-Reported Errors in Electronic Health Record Ambulatory Care Notes. JAMA Network Open. 2020 Jun 1;3(6):e205867-.
Blease CR, Bell SK. Patients as diagnostic collaborators: sharing visit notes to promote accuracy and safety. Diagnosis. 2019 Aug 27;6(3):213-21.


