Dementia
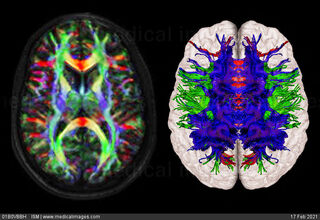
Why White Matter Matters: Diffusion Tensor Imaging
Diffusion tensor imaging helps explain psychoses and dementia.
Posted February 16, 2021 Reviewed by Kaja Perina
What is diffusion tensor imaging?
Diffusion tensor imaging (DTI) is a relatively new magnetic resonance imaging (MRI) technique designed to estimate the axonal organization of the brain via anisotropic diffusion. Axonal matter refers to the white matter in the brain. DTI utilizes thermal Brownian motion of water molecules to assess axonal organization, with the idea being that water molecules diffuse more freely in the main direction of the axons, rather than across them. The maximum amount of diffusion across white matter tracts is projected in the final image.
Why Is DTI important?
Unlike more static methods of brain imaging, DTI is able to capture imaging of the central nervous system (CNS) as well as other complex organized systems outside the CNS. DTI allows us to know the location, orientation and anisotropy of white matter tracts. Cerebral white matter specializes in connectivity, making it essential for completing most mental and behavioral tasks. Specifically, white matter unites regions of the brain, culminating in performances of various mental processes and operations. Disruptions to white matter can therefore result in stark disturbances in behavior and typical mental functioning. The underlying philosophy is that the cortices act in concert to perform various behaviors and mental tasks, and thus it is possible that diagnoses such as schizophrenia — which are marked by dramatic deviations of thought and behavior — are likely the result of white matter deficits.
Clinical Applications of DTI in Schizophrenia and Related Psychoses
Macroscopically, white matter is comprised of various fiber collections such as association fibers, projection fibers, and commissural fibers. For higher order and executive functions (i.e. more complex mental and behavioral tasks) association fibers and commissural fibers are essential. Association fibers travel within individual cerebral hemispheres while commissural fibers travel across hemispheres. Abnormalities in white matter structure and function have been fairly well-documented in cases of schizophrenia and related psychoses. In fact, neurodevelopmental theories of schizophrenia suggest demyelination — or the process by which the myelin sheath that coats axons and speeds their signals atrophies — during childhood and young adulthood is the root cause. In fact, white matter pathology has been noted in individuals with schizophrenia across association fibers and commissural fibers, affecting both cortical and subcortical regions. Not only do these white matter disruptions correlate with psychotic symptoms, but they appear to account for the cognitive deficits noted in schizophrenia as well.
Connecting DTI Use to Schizophrenia and Dementia
Dementia is an umbrella term used to describe diagnoses marked by memory and other areas of cognitive decline. Similarities between schizophrenia and various forms of dementia cannot be denied. This is especially so in cases of behavioral variant frontotemporal dementia, Parkinson’s disease, and dementias secondary to stroke wherein psychotic symptoms are present. DTI has demonstrated that the similarities across diseases do not end at their clinical manifestations, but also persist etiologically in terms of abhorrent white matter pathways. When considering the development of white matter over time, these similarities become more pertinent. White matter, unlike gray matter, does not fully develop until many years after birth, and atrophies at a slow and steady pace in older adulthood (i.e. we seem to have less white matter both at the start and at the end of our lives when compared to gray matter). Both schizophrenia and dementia are marked by an age-dependent onset. It is possible that white matter pathology can account for the psychotic symptoms, cognitive deficits, and age-dependent onset seen in schizophrenia and dementia.
Why Does White Matter (and DTI) Matter?
Beyond its obvious applications of neural mapping and pre-neurosurgical planning, DTI offers us a glimpse into a once undiscovered territory. Until DTI, white matter was not able to be effectively assessed, and so much of its clinical significance was unknown. Given the imperative role white matter plays in severe mental and neurological illness, DTI can elucidate on the nature and causes of diagnoses such as schizophrenia, in the hope that this elucidation can better improve interventions, prevention strategies, and treatment outcomes.
References
Hummer, T. A., Francis, M. M., Vohs, J. L., Liffick, E., Mehdiyoun, N. F., & Breier, A. (2018). Characterization of white matter abnormalities in early‐stage schizophrenia. Early intervention in psychiatry, 12(4), 660-668.
Kelly, S., Jahanshad, N., Zalesky, A., Kochunov, P., Agartz, I., Alloza, C., ... & Yamamori, H. (2018). Widespread white matter microstructural differences in schizophrenia across 4322 individuals: results from the ENIGMA Schizophrenia DTI Working Group. Molecular psychiatry, 23(5), 1261-1269.
Shim, G., Choi, K. Y., Kim, D., Suh, S. I., Lee, S., Jeong, H. G., & Jeong, B. (2017). Predicting neurocognitive function with hippocampal volumes and DTI metrics in patients with Alzheimer's dementia and mild cognitive impairment. Brain and behavior, 7(9), e00766.


