Suicide
Suicide and Lymphoma: My Journey
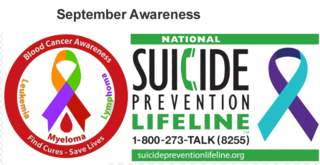
September is Suicide Prevention and Blood Cancer Awareness Month.
Posted September 27, 2019
In light of September’s awareness topics, I wanted to share my personal experience with both suicide and Lymphoma.
Suicide Prevention Awareness
Suicide prevention awareness hits close to home for me. I lost two people whom I loved deeply to suicide, my father and mother-in-law. I was a young child when my father took his own life. After his death, I was told never to tell anyone what happened. I grew up carrying this family secret. The aftermath of suicide for those left behind is profound.
The stigma associated with suicide can make it challenging for loved ones to come to terms with the tragedy and work through their grief. Too often feelings of shame and embarrassment prevent candid conversations about the subject. To this day, there is still much work to do to create awareness and break the stigma associated with suicide.
Even before writing about this experience, I checked in with my siblings. I wanted to make sure they were OK with me sharing this secret. Both were very supportive and encouraging.
As a result of our father’s suicide, both my brother and I, independently, became Thanatologists, specializing in trauma, grief, and bereavement. We couldn’t help our father then, but we want to do what we can now to help others. I have been an advocate for suicide prevention since early in my career. I have written blogs on suicide and suicide prevention. More recently, I wrote a blog about how suicide rates spike in the Spring.
Do you know the suicide warning signs?
Unfortunately, there aren’t always warning signs. However, below are some of the things to look out for to help you determine if a loved one is at risk for suicide.
- Talking about wanting to die or wanting to kill themselves
- Looking for ways to kill themselves, such as online searches or purchasing a firearm
- Talking about feeling hopeless or having no reason to live
- Talking about feeling trapped or in unbearable pain
- Talking about being a burden to others
- Increased use of alcohol or drugs
- Acting anxious or agitated; behaving recklessly
- Sleeping too little or too much
- Withdrawing or isolating themselves
- Showing rage or talking about seeking revenge
- Displaying extreme mood swings
If you, or someone you know, shows any of these signs, especially if the behavior is new, increasing, or seems related to a painful event or loss, please seek help. Call the Lifeline at 1-800-273-TALK (8255) for 24/7, free and confidential support. We can all help prevent suicide.
Blood Cancer Awareness
September is also Blood Cancer Awareness Month. This topic is another that impacts me personally. In 2016, not only was I diagnosed with cancer, but I was told it was one of the strangest forms of cancer my doctors had seen. I was also told if I didn’t undergo a chemotherapy protocol called CHOP, my life expectancy would be about six months. Yet, for many reasons, I chose not to undergo medical treatment. To the surprise of many, I am still here today to tell my story.
Wait and Watch
A tumor on my liver was found during an MRI in May 2014, indicating the possibility of liver cancer. However, I dismissed this at the time, thinking it was a benign growth, much like my benign brain tumor, a meningioma, that was discovered in 2008. In the case of my brain tumor, I made the decision not to undergo brain surgery to remove it unless I became symptomatic.
Instead, we waited and watched. The brain tumor has not grown! I directly attribute this to all I do to take care of myself through my brain rehabilitation program and a brain-healthy diet.
Just like the brain tumor, I decide to wait and watch this tumor on my liver; I had no symptoms of either tumor, and I felt great.
Cancer?
In November 2015, after an MRI, my doctors insisted that I have a biopsy of the liver tumor, which I did in December 2015. This was when I learned that it was not like my brain tumor. The results showed I had lymphoma. Not only lymphoma, but one of the strangest forms ever seen. So strange that I was referred to the chief of oncology who specializes in lymphoma. He had never seen a presentation like mine and agreed that I needed a second biopsy, which I had in February 2016.
The pathology reports clearly showed that the tumor on my liver had four types of lymphoma with the majority being aggressive.
My oncologist wrote the following to me:
“This lymphoma looks aggressive under the microscope, but has acted slow growing. It is similar, but not the same as Hodgkin, treated a little differently. I guess you could say that this is a primary hepatic lymphoma because it is primarily in the liver, but that is not a specific entity.”
Forgoing Medical Treatment
Many people wonder about my decisions to forgo medical treatment. It has a lot to do with a past brain injury and maintaining the life I was able to regain after sustaining a brain injury in 1990. After doctors told me I would not walk or talk again or make any further progress, I took my recovery in my own hands. I overcame many obstacles and found a way to regain my life. Knowing how anesthesia, surgery, and chemotherapy could impact my cognition and possibly undo all of the progress I made after my brain injury, I decided against it.
Several chemotherapy patients I know have experienced months of cognitive issues (memory, thinking, judgment) after their regimens. I lived with these symptoms for almost seven years as a result of my initial brain surgery and concussion, as well as with subsequent concussions and Lyme Disease. No doctor is willing to say I would not have some form of dementia from the chemotherapy.
Yes, the chemotherapy might stop or cure my lymphoma, but I might not be able to function again: I might not be able to write another blog, see patients, or remember my children and grandchildren. I have reached the point in my life where the quality of life was far more important than the quantity of years lived.
The Good News!
Much like coming back from brain injury, I sought alternative methods to treat cancer. I did neurofeedback (pEMF) protocol for cancer, hypnosis (I’m published in the field of hypnosis for cancer), cancer diet, whole food supplements, aromatherapy, and Reiki. Follow-up PET scans showed the tumor decreased in size. This decrease came as a result of absolutely no chemotherapy; it is due solely to my method of treatment. Although doctors thought it was impossible, a newer PET scan shows this tumor is gone. Gone!
That is the good news...
The Bad News
The bad news is that same PET scan showed a new 1 cm tumor on my liver. A later PET scan in April 2019 confirms this tumor, and it shows it metastasized to my lymph nodes, which are three times larger than they were in January. There is also a spot on my lung. I’ve got my work cut out for me again, and I remain hopeful.
The Future
Every four to six months, I have my blood work done. Most recently on September 12, 2019. My blood work is normal, as usual. What is not normal is to have normal blood test results when you have blood cancer, as I do. Yet, neither before my diagnosis nor currently have I ever had an abnormal blood test. This truly is a strange form of cancer.
I have another PET scan scheduled in mid-November to determine the status of my cancer, which is currently at stage 2. In the meantime, I will continue my non-medical treatment methods and stay optimistic. I feel great and am hopeful about the future.
My motto is: There is a way!
You can read more about the alternative methods I used to treat my lymphoma, avoiding chemotherapy, and also follow my journey.
© 2019 DR. DIANE® ROBERTS STOLER, ED.D.




