Autism
A Placental Prognosis for Autism
The placenta indicates risk of autism—and potentially also of psychosis.
Posted April 29, 2013
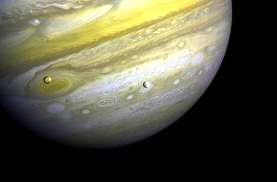
Why do people adopt new and usually—at the time—highly controversial theories? One reason often is that the new theory reveals parts of a bigger picture that the old one never could. Copernicus’s sun-centered model of the solar system is a case in point. The traditional, Ptolemaic universe placed the Earth at the center, with all the other celestial bodies revolving around it. But when Galileo first glimpsed the moons of Jupiter, he realized that he was seeing something that the old Ptolemaic view could not countenance: a separate system of rotation, centered not on the Earth, but on Jupiter.
In many ways, the imprinted brain theory is much the same: a new and utterly simple model that confounds conventional wisdom but opens up perspectives that only it can explain. Take the role of the placenta as a case in point. This is not an organ that figures at all in conventional psychiatry nor normally receives any attention in terms of diagnosis of mental illness. Those who blamed autism on “refrigerator mothers” did not include frigid placentas in the accusation! And even those who advocate a predominant role for genes in autism direct their attention to those expressed in the brain—certainly not to genes in the placenta, and still less to those of the father expressed there.
Yet according to the imprinted brain theory, the placenta is second only to the brain in its significance as an arena for the genetic conflicts that ultimately determine the cognitive configuration of the mind. Indeed, in the paper that first outlined the imprinted brain theory my co-author, Bernard Crespi, cited research published in 2007 that identified a threefold increase in the rate of trophoblastic inclusions (TIs) in the placentas of children with autism spectrum disorder (ASD) compared to children from the general population (Anderson GM, et al. “Placental trophoblast inclusions in autism spectrum disorder.” Biological Psychiatry 61:487–491).
As we pointed out at the time, this is explained by our theory, which implicates paternal growth-enhancing genes in the etiology of ASD. Simply put, the idea is that paternal genes in the fetus get all the benefit of the resources extracted from the mother by the placenta, but pay none of the costs. Not surprisingly then, paternal genes are expressed in the placenta at a level unprecedented in any other organ except the brain, and are directly involved in complications of pregnancy that benefit the fetus at a cost to the mother, such as gestational diabetes (more blood sugar for the fetus) and hypertension (more blood for the placenta to extract it and other resources from).
Now a further and much larger study building on the earlier one points out that the association of increased TIs in the placentas of ASD and at-risk newborns suggests a possible common abnormality that is manifested by increased cellular growth and tissue folding in both the placentas and brains of these children. In children with ASD, the finding of early enhanced brain growth is demonstrated by a steeper than average trajectory in head circumference enlargement during the first year of life, which might reflect augmented generalized growth processes.
However, the new study goes beyond the original one to suggest that placental TIs are a powerful new tool in predicting ASD:
We have identified a marker of abnormal trophoblast proliferation that results in easily identifiable placental TIs, which might be useful to identify newborns who are at risk for ASD. Identification of these children might facilitate very early interventions and improved developmental outcomes at a time when the brain is most responsive to modification. Furthermore, once large cohorts of these infants are identified, improved early diagnostic tools can be developed and tested to hone our ability to further identify which of these at-risk children will go on to develop ASD and/or other developmental abnormalities.
And not only ASD, according to the imprinted brain theory the exact opposite should be the case with psychotic spectrum disorder (PSD), and indeed there is evidence of intrauterine growth restriction, placental undergrowth, and fetal hypoxia in PSD—not to mention smaller brain size, less gray and white matter, and a thinner cortex, as Crespi and I pointed out in our original paper.
The placenta, in other words, takes on a significance for the imprinted brain comparable to that of the moons of Jupiter for the Copernican solar system: it reveals another center of genetic conflict between parental genes apart from the brain which only it can accommodate. Ground-breaking research like that cited here will increasingly urge the cogency of this new, wider view of mental illness, and hopefully offer novel diagnostic tools as its authors suggest—and if the new view is correct, not just for autism, but for psychosis too.
Click here for a video about the PlacentASD™ Test.
(With thanks to Randy Jirtle for bring this to my attention, and to Connie Cho for the link to the video.)


