Addiction
Co-Occurring Mental Illness and Opioid Use: One Family's Story
The Rhodes family discusses their journey to find care for their son.
Posted December 2, 2019 Reviewed by Abigail Fagan
Substance use seldom occurs in isolation. It typically is accompanied by other mental health conditions. This is problematic, given that individuals with co-occurring mental illness and substance use tend to receive incomplete treatment—and incomplete treatment leads to poor outcomes (Avery & Barnhill, 2017).
There are many reasons why clinicians fail to properly treat individuals with co-occurring mental illness and substance use. For one, they feel inadequately trained to work with such individuals. Medical schools and other training programs teach a single diagnosis at a time, ignoring the more common and more perplexing situation of multiple diagnoses (Avery, Zerbo, & Ross, 2016). In addition, once substance use is involved, clinicians may think that other doctors should take over care. At such a point, it is easier to refer to another provider than to continue taking care of the patient themselves.
That said, negative attitudes and stigma towards individuals with multiple disorders may play the largest role in the poor treatment of individuals with co-occurring disorders. Our research has shown that clinicians’ attitudes toward individuals diagnosed with co-occurring disorders may be worse than their attitudes toward individuals with other medical and mental health diagnoses (Avery, Dixon, Adler et al., 2013). And, of course, stigmatizing attitudes are perceived by patients and have been shown to decrease treatment adherence and to worsen psychological distress.
In this blog post, we invite the family of Taylor Rhodes to talk about their son and their journey to find care for his co-occurring disorders.
***
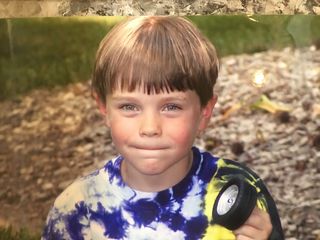
Taylor was a beautiful boy and an out-of-the-box thinker who grasped life’s big picture at a very young age. He loved his friends and his dogs. He loved children and he loved playing sports and video games. His wicked sense of humor brought a lot of laughter to our lives.
Taylor also had an anxious temperament. He was sensitive, a worrier, and felt his feelings in big ways. He was gifted academically, but he struggled with executive functioning and with impulsivity in school. He often found school to be tedious and boring. Taylor’s struggles with anxiety and depression led us to put him on medication in 5th grade.
Towards the end of Taylor’s freshman year in high school, he underwent a sports-related shoulder surgery, after which he was prescribed opiates. This unleashed a beast in his brain, the likes of which we never could have imagined. Taylor would later tell us, once he was in addiction recovery, that when he took those opiates for the first time, his brain suddenly felt “normal.” Unfortunately, he would chase that high, in spite of the costs to himself and to those he loved.
In his sophomore year, a number of developments emerged, which, unbeknownst to us, had Taylor fighting for his life. He began to use Xanax, alcohol, and marijuana, and he was increasingly struggling with anxiety and depression. Because I had been a mental health therapist for more than 20 years and my husband was a director for a large health insurance company, we had a lot of resources at our disposal. I soon realized that none of that mattered.
Trying to navigate the addiction treatment world felt like we had entered the twilight zone. Our son was in crisis, our family was in crisis, and we were trying to navigate a system that was disjointed, siloed, and lacked competent and compassionate care. It was (and is) a system full of differing ideas about what was or wasn’t a good and effective treatment for addiction—and there was a lack of concern for Taylor’s co-occurring mental health issues.
The next several years were consumed with outpatient therapists, group therapy, 12-step meetings, psychiatrists, five inpatient treatment stays, and two therapeutic sober living stays. As parents, we lived in fear every day that we would lose our son—and, in a way, we already had. When he was using, it was like grieving the loss of my son, even when he was standing right in front of me. He wasn’t the boy we had reared and known so well; he wasn’t the brother my daughter had loved so deeply.
A major frustration was the resistance within the clinical and substance abuse treatment community to deal with the anxiety and depression that began in Taylor’s early adolescence. None of the inpatient treatment facilities ever addressed his mental health issues. I went down dead end after dead end trying to reach treating psychiatrists to understand what they were doing to address the mental health issues that I believed were foundational to Taylor’s addiction. He was never placed on medication in any of those facilities. They seemed only willing to address the addiction, regardless of my demands or pleas.
Once a facility or insurance company decided Taylor needed to move along to the next step in treatment (even though my husband and I thought he was often not ready), there was little to no assistance in determining what the next step was or how Taylor would get there. It was on us as a family to figure out that next step, though we were barely able to breathe from the herculean feat of getting him into treatment in the first place.
All too often the clinicians treating Taylor were overworked or, worse, had little or no clinical expertise. When I would ask clinical questions, I was often met with silence on the other end of the line. I was given the run-around about why they weren’t dealing with his mental health issues, but when we considered moving Taylor to yet other facilities, it seemed risky. If he was stable, even if not being treated properly, we worried that moving him could make things worse. We had experienced such poorly run facilities and programs throughout our journey.

Many of the treatment teams during Taylor’s intakes would tell us that he was going to try to manipulate us so he could leave. They recommended that we not believe what he said, but instead should practice “tough love.” In other words, “don’t believe your son.” I am glad that never resonated with us, and we always trusted Taylor’s instincts. To us, “tough love” came to mean loving our child no matter what and walking beside him in the fight of his life.
Sadly, others in the medical community we encountered really didn’t care. They were accustomed to treating individuals and their families like second class citizens. What are people going to do when they are fighting for their lives? I didn’t have time to stop and call out negligence or incompetence or lack of compassion for what it was. I wasn’t ashamed of my son: I knew his addiction was a disease and not a choice or moral shortcoming. We were too busy trying to save our son and get him help and support. That was the only fight we had time for. My biggest regret in all this is that I trusted those who treated Taylor to give us guidance and point us in the right direction. I realize now they don’t know what they don’t know.
On June 29, 2019, sometime after two in the morning, my beautiful boy lost his battle with addiction when he overdosed on heroin laced with fentanyl after 10 months in recovery. Twenty years and 12 days were all we would ever have with Taylor. In an instant, we joined the other 192 people in this country who lose this battle each day. We can all do better and I pray we do. Too many lives are counting on it.



References
Avery J, Barnhill J. Co-occurring Mental Illness and Substance Use Disorders: A Guide to Diagnosis and Treatment. Arlington, VA: American Psychiatric Publishing, 2017.
Avery J, Zerbo E, Ross S. Improving Psychiatrists’ Attitudes Towards Individuals with Psychotic Disorders and Co-Occurring Substance Use Disorders. Academic Psychiatry. 2016; 40(3):520-22.
Avery J, Dixon L, Adler D, Oslin D, Hackman A, First M, Goldman B, Koh S, Nossel I, Siris S. Psychiatrists’ Attitudes Towards Individuals Diagnosed with Substance Use Disorders and Serious Mental Illness. Journal of Dual Diagnosis. 2013 October; 9(4):322-326.




