Sleep
Too Many Sleeping Pills!
A patient's struggle with a shopping bag full of pills
Posted September 15, 2013
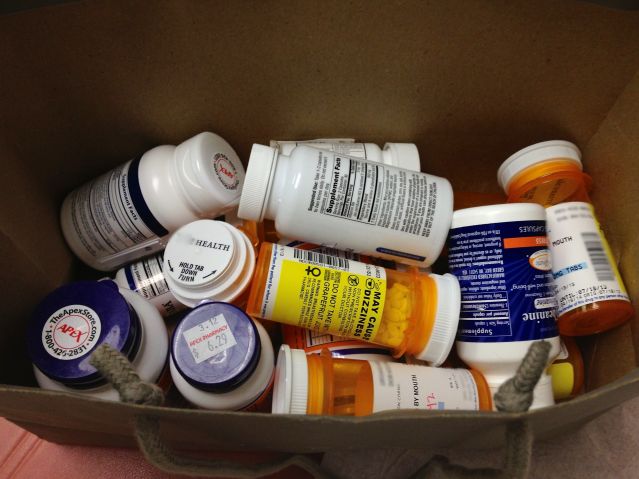
It terrifies the clinician when a patient brings in a shopping bag full of pills.
Radio Silence but Busy Putting Book to Bed
I have not posted to this blog in about three months because I have been busy completing my latest book, Atlas of Clinical Sleep Medicine. One of the most gratifying days in the life of an author is when all of the page proofs have been approved, when files of final pages are shipped off to the printer, and within three to four months magic happens when the book is launched. It does not matter whether it is one’s first book or tenth book, bringing a book to life is very satisfying. However, life goes on and clinics continue, and I am still challenged with often difficult cases.
Terrifying Sight
One of the sights that terrifies some doctors is when a patient comes to a consultation bringing a shopping bag containing vials of pills; some purchased over the counter, some prescribed, and some as health food supplements. I was dumbstruck recently when I saw the above shopping bag, because the patient looked so healthy. She reassured me that this bag contained only the medications she used to help her sleep, but ultimately she wanted to be off the medications and was referred to me for an opinion about how to achieve that. Her insurance company had authorized one visit. Quite a challenge for a one-hour office visit.
Thirty Years of Insomnia
The patient was a single woman, 50 years old, with a history of insomnia going back to age 20. Since that time the overall pattern has remained the same. She would have no difficulty falling asleep, and about one to two hours later she would abruptly awaken, her heart pounding, and then find it difficult to fall back asleep. At times she would lie awake for the rest of the night and would become anxious about not sleeping. She would often become hot and sweaty, with the back of her neck and hairline drenched, and her pajamas, pillow cases and sheets sometimes wet. As she was trying to sleep, her legs shook uncontrollably and seemed to move on their own. She would find some relief by massaging them or even walking. However, the longer she was awake, the more distressed she became about not sleeping. She could not turn off her racing mind.
Over the years, she had tried unsuccessfully all the "damned" sleeping medications available. These included prescribed hypnotics (medications approved by the FDA to treat insomnia), antihistamines, anti-depressants, and even medications used to treat schizophrenia. None of them worked. The healthy appearing woman was currently taking 13 prescribed medications and probably an equal number of health food supplements that she thought would help her sleep. She was seeing several doctors and needed a diary to keep track of all her appointments. She didn’t want to use sleeping pills, only supplements, which she felt were safer. But here she was, going back to the supplements she had been using and she still had near-middle of the night insomnia.
Furthermore, this patient had been diagnosed with anxiety and depression, was on antidepressants, and was taking anti-anxiety medications as needed, mostly at night before bed. For more than 20 years she had been taking thyroid hormone replacement because she has a “low thyroid.” As a teenager she was told that she had anemia after she started menstruating. And although she bled a great deal with her menstrual cycles, she had never been treated with replacement iron. She was not yet menopausal.
Treatment for depression and anxiety were not having a positive effect on her sleep. Her psychiatrist was treating her anxiety disorder with a short-acting, anti-anxiety medication at bedtime. All her medications, in all sorts of combinations, did not prevent her from waking up. She never actually had trouble falling asleep.
Where to Begin?
After hearing all of this, my mind whirled with several possibilities. Perhaps she was taking too much thyroid hormone, since insomnia and night sweats are common with hyperthyroidism. She had symptoms of restless legs syndrome. The cause of this could have been chronic iron deficiency, or even a side effect of an anti-depressant medication.
I recommended that her thyroid status rigorously be re-assessed, since by her clinical history she never had any symptoms of hypothyroidism and for decades prescriptions were merely being refilled. I recommended that her iron status be assessed. I was fairly certain that her iron stores are low based on her history, and that replacement iron would help the restless legs symptoms that she had in the middle of the night.
I recommended that her primary care practitioner review every one of her thirteen prescribed medications and to document a reason why they were started and whether there was current justification for her to be on them. In my opinion, there is hardly ever a justification for an otherwise medically healthy person to be on so many medications, especially when the medications are not having their intended effect.
I recommended that she be referred for cognitive behavioral treatment for insomnia. Her inability to shut off her racing mind in the middle of the night I believed was an important factor perpetuating her insomnia. Her psychiatrist did not do cognitive behavioral therapy, a treatment that is frequently very effective in patients, especially those trying to wean off of their medications. (There is an entire chapter about cognitive behavioral therapy in my ebook The iGuide to Sleep .) He felt that cognitive behavioral therapy, administered by an experienced psychologist with experience in treating insomnia, would be the most important plan in her long-term treatment.
I learned several days later that her medical insurance company denied the request for cognitive behavioral treatment for insomnia. Her plan did not cover such psychology services. The patient was heartbroken.
How ironic. Her insurance company has paid many, many thousands of dollars over the years on medications and doctor visits which did not help her. Her insurance company whose professed goal is to keep their beneficiaries healthy would not pay for the one thing that her psychiatrist and I both thought would make the biggest difference in her life.
Sometimes there isn't much that one can achieve in a one-hour visit that makes up a minuscule portion of a single patient's 30-year struggle in a broken health care system that is negatively impacting millions of lives every single minute. How many people have shopping bags full of vials of pills because they are denied treatment that could help them?




