Coronavirus Disease 2019
Why Am I So Tired?
Managing fatigue during the COVID-19 pandemic.
Posted February 13, 2021 Reviewed by Ekua Hagan
This post was written by Dr. Robert M. Gordon, Dr. Joanna B. Wolfson, and Elina Talis. Dr. Gordon is a member of the Hospital, Healthcare, and Addiction Workers, Patients and Families working group of the COVID-19 Psychology Task Force (established by 14 members of the American Psychological Association) that sponsors this blog.
Fatigue in the General Population Due to COVID-19: The Stress Response
Numerous factors have made the COVID-19 pandemic stressful and potentially traumatic for individuals. People have now been facing unprecedented stressors for close to a year due to illness or loss, fear of getting sick or infecting others, social isolation, and significant lifestyle, job, or school changes. While vaccine distribution offers promise for individual immunity, there is protracted uncertainty about the duration of the crisis and its psychological, economic, political, and societal consequences.
As clinicians in a large health care setting, we have heard many versions of the phrase, “I’ve just been so tired lately.” Patients and colleagues alike are alluding to a fatigue that may be unfamiliar—leading some to question whether the pandemic is taking a physical toll, even if not subjectively experienced as an acute, anxiety-provoking experience.
With extensive or prolonged stress, the body can experience physical and emotional exhaustion.
Most people are familiar with the term “fight or flight,” in which you detect some type of threat (e.g., almost stepping into oncoming traffic) and the body quickly goes into protective mode: heart rate increases, muscles tense, blood pressure rises, and vision focuses. This quick and automatic physiological response occurs so that we can run away, fight back, and survey our surroundings.
These responses to threat are usually brief and over once we fight or flee. In fact, the stress response is only meant to last a short period of time given as the body is flooded with adrenaline and cortisol which are generally only present in smaller quantities. However, with a more continuous threat such as the pandemic, this stress response can be playing in the background, out of our awareness, and start to weigh on physical and emotional well-being. In fact, this response is so automatic that its default mode is to give us the hormones and oxygen reserves we need to run, jump, or fight back. When these go unused, the result is dizziness, muscle tension, and exhaustion.
High levels of stress can also cause our bodies and minds to become so overwhelmed that our systems shut down. Some people actually become so fatigued after experiencing a threat that they immediately lie down and go to sleep.

Fatigue in Health Care Workers
Compassion fatigue refers to emotional exhaustion from working with a traumatized population and is a form of caregiver burnout (Figley, 2002). The model is based on the assumption that empathy and emotional energy are driving forces in effective work with suffering, but there is a physical and emotional cost.
Compassion fatigue limits our ability to bear others’ suffering: it can lead to emotionally zoning out or avoiding triggers of patients’ traumas. Stories abound of overwhelmed hospital systems due to COVID-19 and medical workers having to move from patient to patient in similarly dire situations. It is not unusual to feel numb in this environment.
Individuals typically interpret new information on the basis of unquestioned assumptions and expectations about themselves and the world including the illusion of invincibility and invulnerability. Traumatic events undermine these premises. Health care workers can no longer feel that "the world is just” and "individuals can control the world and minimize their vulnerability through their own behavior.” These assumptions need to be revised on the basis of the pandemic to "the world is often a random place and bad things happen for no reason" (Hill, 2018; Janoff-Bulman, 1989).
Fatigue in Patients Who Contracted COVID-19
Fatigue is highly prevalent in patients with post-COVID-19 infection. A study by Townsend et al. (2020) revealed that more than half of the patients reported persistent fatigue 10 weeks after initial symptoms. Fatigue was not associated with COVID-19 severity, such as the need for inpatient admission, supplemental oxygen, or critical care. Similarly, Mandal et al. (2020) found that roughly 69% of patients reported fatigue post-discharge.
Tips for Fatigue and Stress Management
Stress Management Techniques
-
Use relaxation tools, such as deep breathing and mindfulness
-
Pace yourself and make space: take breaks, get sunlight, separate work and home life
-
Set realistic expectations: try not to compare yourself to your pre-COVID self; break larger goals into smaller, more manageable steps with clear time frames
-
Connect with your support system, but put limits on how much time you spend discussing COVID-19-related issues with others
-
Follow an information diet: limit exposure to upsetting news and social media
-
Seek help from a mental health professional, especially if anxiety or depressed mood feel unmanageable, distressing, or impact daily functioning
Healthy Sleep Techniques
- Stick to a consistent sleep schedule
- Develop a soothing bedtime routine
- Protect the bedroom for sleep and intimacy, rather than as a workspace
- Limit the use of screens and electronics before sleep
- Avoid caffeine too late in the day/limit substance use
Strategies for Dealing with or Limiting Compassion Fatigue
- Recognize the symptoms of compassion fatigue
- Talk to colleagues and professionals
- Have self-compassion: direct kindness, understanding, and acceptance toward yourself
- Identify what is meaningful. Questions such as “What gives you a sense of purpose?" and "What do you look forward to doing when the pandemic is over?” can be catalysts to gaining awareness of meaning in life (Hill, 2018).
- Reevaluate values and priorities
- Foster self-care: enjoy nature and schedule time to pursue creative outlets or hobbies
Concluding Thoughts
Fatigue is a main symptom of the pandemic for many, whether as a patient, frontline worker, or member of the general public. This might be inescapable given what we know about the stress response and the costs of caring and empathy, but multiple strategies can be beneficial.
Although decidedly challenging and physically and emotionally draining, a potentially positive result of dealing with COVID-19 has been the opportunity to reflect on assumptions, values, priorities, and what is most meaningful in life, and living life with a greater sense of urgency, intention, and purpose (Gordon et al., 2020).
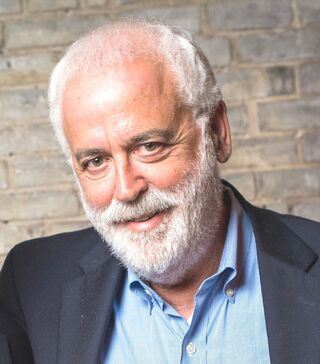
Robert M. Gordon, Psy.D., is the Director of Intern Training and Associate Director of Postdoctoral Fellow Training at Rusk Rehabilitation and Clinical Associate Professor at NYU Grossman School of Medicine. He received his doctorate from Ferkauf Graduate School of Psychology. Dr. Gordon has specialties in the areas of neuropsychological and forensic testing and psychotherapy with children and adults with physical and learning disabilities and chronic illness. He has published in the areas of ethics, supervision, existential-humanistic and relational approaches during COVID-19, dream interpretation, pain management, and the use of projective testing in neuropsychology. Dr. Gordon is a member of the COVID Psychology Task Force (est. by 14 divisions of the American Psychological Association working group: Hospital, Healthcare, and Addiction Workers, Patients and Families that sponsor this blog.

Joanna B. Wolfson, Ph.D., is a Clinical Instructor of Rehabilitation Medicine at NYU Grossman School of Medicine and a Senior Psychologist at NYU Rusk Rehabilitation. She received her doctorate from Fairleigh Dickinson in Clinical Psychology. Dr. Wolfson completed her internship at Rusk Rehabilitation and postdoctoral fellowship at the Manhattan VA in health psychology/primary care. Her special interests include behavioral health interventions, and CBT for mood/anxiety difficulties related to TBI, vestibular conditions, and other medical illnesses.

Elina Talis, MA is a Psychology Intern at NYU Rusk Rehabilitation. She is currently completing her doctorate of psychology at William James College in Massachusetts with an emphasis in Clinical Neuropsychology. Her research interests include accelerated memory loss, the cognitive profile of autoimmune encephalitis, and the integration of technology with mental health.
References
Figley, C. R. (2002). Compassion fatigue: Psychotherapists’ chronic lack of self-care. Journal of Clinical Psychology, 58(11), 1433–1441. https://doi.org/10.1002/jclp.10090
Gordon, R. M., Dahan, J. F., Wolfson, J. B., Fults, E., Lee, Y. S. C., Smith-Wexler, L., Liberta, T. A., & McGiffin, J. N. (2020). Existential-humanistic and relational psychotherapy during COVID-19 with patients with preexisting conditions. Journal of Humanistic Psychology. Published online: November 2020. https://doi.org/10.1177/0022167820973890
Hill, C. E. (2018). Meaning in life: A therapist’s guide. American Psychological Association. http://doi.org/10.1037/0000083-000
Janoff-Bulman, R. (1989). Assumptive worlds and the stress of traumatic events: Applications of the schema construct. Social Cognition, 7, 111-136. https://doi.org/10.1521/soco.1989.7.2.113
Mandal, S., Barnett, J., Brill, S. E., Brown, J. S., Denneny, E. K., Hare, S. S., Heightman, M., Hillman, T. E., Jacob, J., Jarvis, H. C., Lipman, M. C. I., Naidu, S. B., Nair, A., Porter, J. C., Tomlinson, G. S., & Hurst, J. R. (2020). ‘Long-COVID’: A cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalization for COVID-19. Thorax, thoraxjnl-2020-215818. https://doi.org/10.1136/thoraxjnl-2020-215818
Townsend, L., Dyer, A. H., Jones, K., Dunne, J., Mooney, A., Gaffney, F., O’Connor, L., Leavy, D., O’Brien, K., Dowds, J., Sugrue, J. A., Hopkins, D., Martin-Loeches, I., Ni Cheallaigh, C., Nadarajan, P., McLaughlin, A. M., Bourke, N. M., Bergin, C., O’Farrelly, C., … Conlon, N. (2020). Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLOS ONE, 15(11), e0240784. https://doi.org/10.1371/journal.pone.0240784




