Trauma
PTSD: An Unconscious Choice to Stay Alive
A self-regulation exercise for PTSD Day.
Posted June 30, 2021 Reviewed by Ekua Hagan
Key points
- PTSD stress reactions are an unconscious choice made by your nervous system to stay alive.
- Dysregulation is at the core of PTSD. This manifests as chaos in multiple systems of human functioning.
- Trauma affects all aspects of wellness: emotional, cognitive, physical, social, and spiritual.
- Self-regulation in trauma therapy should include experiential psychoeducation and a step-by-step process to facilitate body awareness.

Life after trauma is complex. Many survivors struggle with a daily sense of being overwhelmed by life and by emotions that are difficult to control. For therapists, helping clients self-regulate is a priority, especially those with PTSD.
In support of PTSD Day, in this post I review key understandings of self-regulation that therapists need in order to work with trauma survivors with PTSD and suggest strategies for doing so. Near the end, I also include a short video demonstration of one of the therapeutic tools I use in working with clients on self-regulation.
Dysregulation Is at the Core of PTSD
A common consequence of trauma is an overall sense of dysregulation. This manifests as chaos in multiple systems of human functioning. During a traumatic event, emergency protective processes are activated. Instinct and autonomic fight/flight and freeze responses take over; rationality, thought, and powers of conscious choice are shoved aside. The more threatening the survivor's nervous system perceives the event to be, the more automatic the reactions are, and the less control the survivor has over the reactions, both in the moment and later. (more on this in part 1, part 2).
In the immediate aftermath of a trauma experience, survivors suffer from stress symptoms such as a racing pulse, hyperventilation, nausea and/or vomiting, trembling and shaking, uncontrollable crying. (Some forms of trauma, notably developmental trauma, may not necessarily be easily traceable to a specific event.)
Whereas early reactions gradually fade in most cases, for survivors with PTSD, the sense of unpredictability that follows lasts for months or years. The effects are pervasive and invasive, for all systems are involved through neural pathways and imprints that are not easily accessed or managed by rational thought:
- Emotional – Trauma typically sets off endless cycling through emotions of shame, guilt, fear, anger, and pain.
- Cognitive – Trauma affects the ability to process thoughts, memory. It also affects attention, focus, retention, and the ability to use reason.
- Physical – It affects the functioning of muscles and joints, metabolism, temperature, sleep, immune system, etc.
- Spiritual – Trauma affects worldview, that is, a survivor’s understanding of life, purpose, and meaning.
- Social – Trauma affects relationships with spouses, family, friends, colleagues, and strangers.
As a result, many survivors feel “on edge” and overwhelmed most of the time, with all inner resources consumed in a struggle to cope with the constant sense of lack of control they carry. They are chronically stressed, and over time, they become burdened by chronic stress symptoms that may include fatigue, insomnia, immune dysregulation (getting sick easily), a pervading sense of overwhelming sadness, numbness (different levels of dissociations), rumination, and so forth.
Self-Regulation Post-Trauma
Self-regulation refers to the ability to maintain control over one's sensory, emotional, and cognitive reactions. Everyone needs to learn and practice self-regulation in order to maintain a sustainable life and experience life-giving relationships with self and others. This is far from easy and most people struggle with self-regulation at various points across all phases of life.
For trauma survivors, the challenges are harder. Their wounds make them hyper-reactive. In addition, they are often fatigued, emotionally and physically, by the endless struggle to cope with their reactions.
However, for the same reasons, the rewards of expanding capacity for self-regulation are high. Because it is such a daily struggle, survivors take immediate note of progress in this area and are greatly encouraged by it. As they begin to experience patterns and predictability in their coping responses, they gain renewed access to the inner resources of hope and courage that seem to be part of the human birthright. Progress in self-regulation lays a foundation for progress on other problems.
Two Manifestations of Dysregulation
Dysregulation after trauma manifests in two opposite ways. Some survivors are prone to hyperarousal, which is like carrying an invisible volcano inside, stoked with easily triggered anger, panic, or anxiety. Other survivors are prone to the opposite, hypoarousal, characterized by numbness.
A common pattern is that survivors experience hyperarousal for a time just following the traumatic event. Then, overwhelmed and exhausted, they shift into hypoarousal. Such dysregulation is temporary for some survivors and prolonged for others (more on this in part 1 and part 2).
Self-Regulation Is Key for Trauma Integration
Though improving self-regulation is an early goal in therapy, a carefully planned and ordered procedure for working on it is essential. The client’s sense that life is unsafe, unpredictable, and unsustainable is a huge obstacle. Clients need concrete experience that the therapeutic relationship is the opposite.
A clearly conceived therapeutic framework is essential to understand and address the stress symptoms. As we execute this plan, it’s essential to do so in ways that help clients to feel safe and that the therapist is predictable and reliable. The goal is a growing sense of attunement between client and therapist as two key therapeutic activities take place:
1. Psychoeducation
Helping survivors regain or invent a new sense of self-regulation is a slow, sequential process that usually begins with psychoeducation about the differences between emotions, feelings, and sensations (more in this post).
This psychoeducational foundation is important, for it provides context and definitions relevant to the world of a client’s own experience. Such knowledge alone is remarkably calming, empowering, and stabilizing for many clients.
In addition to its intrinsically stabilizing contribution, psychoeducation lays a foundation for the critical work ahead. Once the client has a grasp of the general terms, the differences between emotions, feelings, sensations, and how each applies to the client’s context and personal manifestations of symptoms, we can then begin to work with therapeutic modalities that enhance body awareness.
2. Body Awareness
This means learning to detect and trace what is happening in the body. Humans are embodied creatures — our experience of self and reality is mediated through the body. Since trauma responses are so pervasively and uncontrollably experienced in the body, work with the body is by far the most direct and powerful way of addressing them.
But because it is both direct and powerful, work with the body with trauma survivors is like touching a live wire. Careful preparation and an incremental approach are required.
A good place for early body awareness work is with a review of what sensations a client associates with various triggers, emotions, movements, images, etc.
Modalities to facilitate body awareness include:
- Grounding (bringing awareness simultaneously to what we experience in the body and to connecting to ground/earth).
- Embodiment (bringing awareness of the body to the act of noticing sensations)
Therapeutic modalities that assist in the development of body awareness include expressive therapies (arts, drama, movement, dance, music), body-oriented therapies, certain mindful modalities, and certain neurofeedback protocols.
A commonality of these modalities, when properly deployed in trauma therapy, is that although they may include the use of talk to process the dynamics of therapy, they do not rely on cognitive processing as their primary mechanism of impact. See the video for an example of a hand-tracing body awareness exercise.
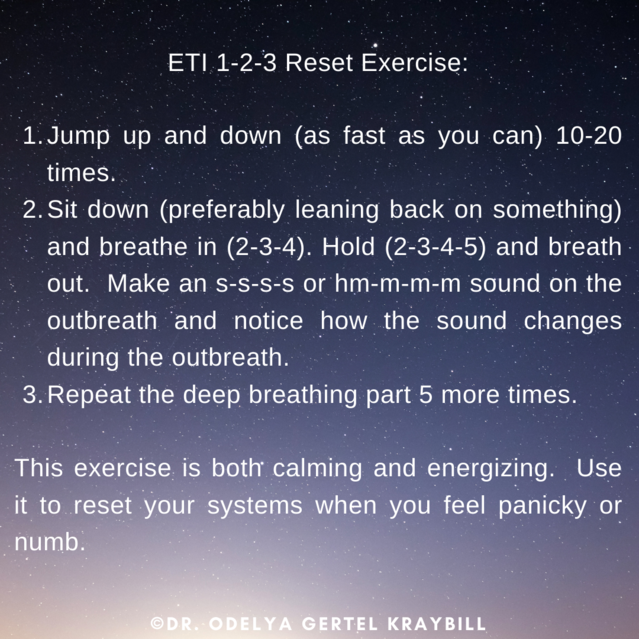
It is important to note that the exercise in the video is a short example of a step-by-step “how-to” process for learning self-regulation. This process must be conducted with utmost attention to safety and predictability for the client. Engagement with the body requires preparation. Without preparation, it can lead to instant resurfacing of symptoms and possible retraumatization. Therapists, therefore, need to think carefully about any bodywork, anticipate possible associations, make sure there is session time available to deal with whatever may come up, and prepare therapeutic strategies for coping. Use the reset exercise (see image below) if your client is too overwhelmed.
This post is introductory in nature and gives only a quick overview of the role of self-regulation in therapy. The Expressive Trauma Integration (ETI) self-regulation protocol is a mix of psychoeducational theory and many different practices designed to help therapists work systematically with clients in establishing emotional regulation. For more in-depth information about the framework see here.
Early in work with survivors, and repeatedly throughout, I try to give my clients insight into the origins of the trauma symptoms that so disturb their life and sense of well-being. I often say things something along these lines:
The body’s response to trauma is a highly refined response designed to keep us alive. Your trauma responses are actually ancient survival tactics that helped your ancestors to react instantly in the face of grave danger, to fight fiercely or to run quickly away, and to monitor the environment constantly for any new signs of danger. If your ancestors hadn’t honed these responses to a sharp edge, you might not be here today.
Many survivors are better able to live with and manage trauma symptoms when they understand them as part of a response system that plays a central role in human experience. As we work with your experiences, you may find it helpful to remind yourself that at their core, these stress symptoms represent a powerful will to stay alive, passed down to you by your ancestors and powerful still today in you.
To find a therapist, please visit the Psychology Today Therapy Directory.




