Depression
Brain Networks in TMS for Combined PTSD and Major Depression
New TMS research provides insight into how to refine existing approaches.
Posted January 15, 2018 Reviewed by Abigail Fagan
Everything we do, every thought we've ever had, is produced by the human brain. But exactly how it operates remains one of the biggest unsolved mysteries, and it seems the more we probe its secrets, the more surprises we find. —Neil deGrasse Tyson
Transcranial magnetic stimulation (TMS) uses repeating strong magnetic pulses to change the activities of neurons. TMS gives us the ability to directly influence brain activity in a highly selective manner, enabling an unprecedented degree of control over how our minds function—for clinical and other applications (e.g. forensic, performance enhancement, etc.).
When applied across the skull to different areas of the cortex of the brain, TMS can have varying effects. The effect of the TMS depends on what areas are targeted, including the depth into the brain, whether the stimulation is used to increase or suppress activity in that area, and how changing activity in that brain area affects the overall function of the brain, and the subjective experience of the individual. As TMS therapy has been officially used in the U.S. since 2008 for the treatment of major depressive disorder unresponsive to at least one medication, using a rather basic protocol, the future use of TMS (and related neuromodulation techniques such as transcranial direct current stimulation, tDCS) will depend on developing more sophisticated understanding of how the brain works.
By forcing neurons to fire using a moving magnetic field to push electrical charge within the cells themselves, the overall activity of the brain can be shifted from one state to another, in some cases. Thus it is possible to shift the brain from a depressed to a healthy pattern, or shift patterns of disordered cognition or emotion processing in PTSD to restore proper function, or slow down activity in motor areas in the brain to interfere with hyperactive circuits in obsessive compulsive disorder, or reduce activity in the auditory cortex to quell hallucinations, and so on. Understanding the brain from a network point of view provides the information required to design better treatment protocols and build more accurate models and sims.
Traditionally, brain function has looked at the biology and electrophysiology of neurons, and used anatomic studies with basic imaging to determine whether there are differences in size in different parts of the brain or differences in activity or pathology in neurons, and so on. Given the penetration of systems theory and related mathematical modeling into every field and neuroscience’s close relationship with mathematics and psychology, the application of network theory to understanding how the brain works has begun to close the gap between mind and brain. Advances in functional neuroimaging techniques and mathematical modeling allow for a deeper window into not only how the brain works, but how to make the brain work the way it ought to work (in cases where there is a clear function and dysfunction) when the system is considered pathological. Even at an early stage of development, neuromodulation tech like TMS gives clinicians the power to directly try to correct pathological brain activity.
The current study is of note for collecting data on the clinical response and network impact of using TMS to treat patients with both Major Depressive Disorder and PTSD. Early studies in any field tend to look at simplified situations, and TMS studies have mainly looked at people with one condition or another, excluding people with more than one condition from studies. As PTSD and depression often are co-morbid, this study is more relevant for working with actual clinical populations where people very often have two or more co-occurring medical-psychiatric conditions. Depression and PTSD are both more common in many groups, including those with early adversity and higher levels of later-life stress. We want to know what TMS protocol will work best for which patients, and that requires (among other things), studying TMS in different groups. While conventional treatments are helpful, they don’t work at all for a significant percentage of patients, and for others work to a limited extent or have undesirable or unacceptable side effects. New treatments are required to address this lack of effectiveness.
Brain networks
There are a few things to know before understanding the study, which goes into great detail. First of all, what are we talking about when we say “brain networks”? There are several brain networks, but three of special interest in both PTSD and depression are the executive control network (ECN), the salience network, and the default mode network. All brain networks represent activity among interconnected physical regions of the brain firing in a complicated dance in a constant flux of activity. Networks, as such, are not specific brain areas but a functional cluster of linked regions akin to the hardware of a computer network.
The ECN directs the brain and regulates emotions, the salience network picks out what we notice internally and externally, and the default mode network is the brain’s resting state. They have all been found to be altered in different ways in both depression and PTSD, with a long list of observed changes in different brain regions, and sometimes confusing or conflicting results. Functional imaging allows researchers to look at brain network activity and construct a picture of what brain networks look like in different clinical conditions, and compare pre- and post-treatment imaging with healthy brain networks to determine what happened in the brain as a result of an intervention.
The current study
Based on past research and theory, Philip, Barredo, Wout-Frank, Tyrka, Price and Carpenter (2018) used TMS to treat the right dorsolateral prefrontal cortex (DLPFC) at a frequency of five pulses per second, over the course of one session (usually 30-40 minutes) delivering a total of 3000-4000 pulses in separated trains of pulses each a few seconds long. Imagine a slow woodpecker tapping on and off a few times every couple of minutes. Each patient had around 36 sessions, over the course of several weeks.
The DLPFC is a standard treatment site for depression, and is an important component of the ECN, which has been shown to have abnormally low activity in both PTSD and depression. If the ECN isn’t strong enough, for example, it can’t shift the salience network away from fixating on negatives toward more positive, forward-looking views, causing ongoing problems. One important purpose of the study was to develop predictors for treatment response to guide future treatments as combined PTSD and Major Depression is difficult to treat, leading to chronic suffering for too many.
They treated to completion a total of 26 people (39.3 percent women, average age 51) who met diagnostic criteria for both conditions. They were depressed and had PTSD from physical assault, sexual assault and abuse, and driving accidents, mainly. Researchers collected before and after brain imaging using functional MRI, as well as data on clinical response. They looked at differences among anatomic regions, and calculated changes in connectivity between them. The results are very detailed but major findings stand out.
The Findings
One-third of participants with both PTSD and depression met criteria for a significant clinical response as measured by standard scales (PCL and IDS-SR, for PTSD and depression, respectively). This is lower than for either condition alone, but not surprising given the greater severity of illness and history of poor response to prior treatments. For someone who has failed to respond to prior standard treatments (usually psychiatric medication and psychotherapy), TMS can offer substantial relief to a significant fraction, without high risk of major adverse reactions. A moderate improvement in chronic burden of illness can translate to a big increase in quality of life and function.
Using their network-based approach, they found that a key area with abnormal activity across many conditions, including those treated in this study, is the subgenual anterior cingulate cortex (sgACC). They found that altered connectivity of the sgACC within the default mode network (DMN) predicted response to TMS in this group. The sgACC is a highly connected node important in many brain functions, involved in regulating fear reactions leading to adaptive or maladaptive responses to threat, suppressing emotions required to properly function in personal and social spheres, and regulating reward circuits to sap motivation, drive appropriate goal-directed behavior, or lead to excessive, manic activity when too active (Drevets et al., 2009).
TMS response was also predicted by increased connectivity between the prefrontal cortex (the PFC, a broad anatomic area, containing components of the executive network) and the amygdala, which is important for strong emotions and fear responses to threat. The amygdala is closely connected with regulating the hippocampus, involved in memory, narratives and placing experiences within the appropriate context to avoid disagreement between internal experiences and external reality. The PFC is composed of sub-regions, and different areas may be connected to the amygdala differently. Areas of the PFC serve different functions, and over-connection with fear centers would lead to different symptoms depending on which areas.
In their discussion, the study authors report that “the present findings suggest a relationship between the degree of network pathology and treatment outcome, and that a ‘healthier’ signature of network connectivity (characterized by a less hyperconnected DMN and greater PFC-to-amygdala connectivity) predicted TMS response.” Patients with low connectivity between key areas of the PFC and amygdala may not respond well to TMS, as the path between the cortex and the deeper brain region has to be available for stimulation in order to amp up activity in the targeted networks. Patients considering TMS could be imaged for network activity first. In principle, those with intact anatomy in principle could be converted to TMS responders by pre-treating them with another neuromodulation approach, such as tDCS, or possibly other therapeutics including medication changes, neurofeedback, or psychotherapy. On the other hand, if pre-TMS testing revealed physical damage, such as anatomic lesions as from traumatic brain injury or pathology from autoimmune or neurodegenerative disease (for example), it would not be possible to increase connectivity without addressing the underlying damage. It is possible to imagine “patching” different brain regions together with implants to compensate for damaged pathways using microtechnology.
Predicting response to TMS
For those who responded to TMS in this study, there were two major markers of clinical response. First TMS decreased connectivity between the sgACC and the DMN (default mode network), and decreased connectivity between the hippocampus and the SN (salience network). There were also sgACC connectivity changes with areas of the prefrontal cortex (PFC) including medial PFC and dorsolateral PFC, both important for different functions related to depression and PTSD and found to be important in earlier research. Though it is sometimes too easy to fit observations to our expectations, these findings make sense given that people with PTSD and depression may fixate less on negatives (and therefore experience greater cognitive flexibility and neuroplasticity) if the sgACC is no longer driving us (via the DMN) to dysfunctionally ruminate on problems when we are idle.
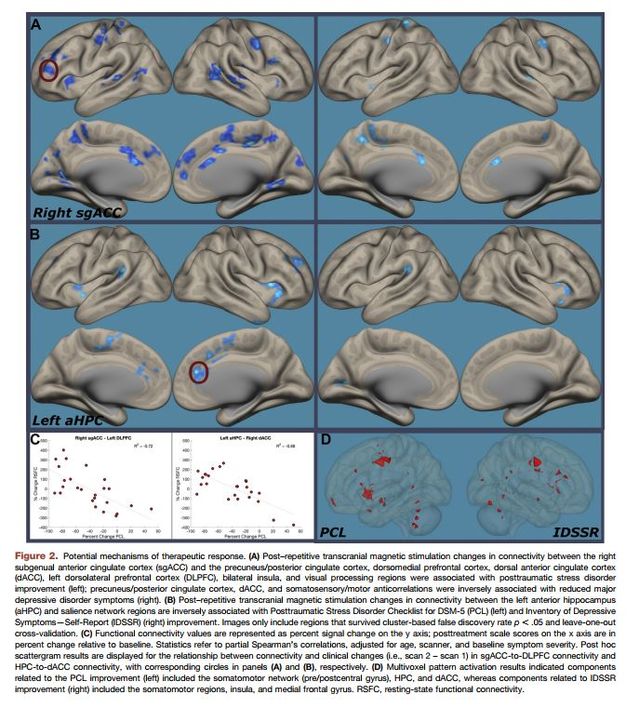
Likewise, decreased sgACC input to the hippocampus and SN would be expected to alleviate aspects of both PTSD and depression symptoms by allowing for both better contextualization of experiences and emotions, improved memory function especially regarding positive vs. negative views of oneself and others, and greater ability to shift attention from distressing thoughts or negative past experiences toward more adaptive and helpful considerations. Changes of this nature parallel improvement in or recovery from symptoms of depression and PTSD, and moreover represent arguably a normalization of broad patterns of brain activity more consistent with living more fully and functioning more effectively, feeling better about oneself, and getting along better with others.
Future directions
TMS is still early on in its development, though since being FDA-cleared for Major Depression in 2008 in the U.S. has become a standard treatment while it is being refined. Studies such as this one which investigate TMS response and predictors will help to guide future clinical practice, and allow the translation of neuroscience research into treatment protocols which target networks involved in depression, PTSD and other conditions. Other avenues for TMS development include using different patterns of magnetic pulses, using different types of magnetic coils to reach deeper areas of the brain, combining TMS with other approaches to prime for better responses, and treating multiple brain regions for greater impact to benefit treatment-resistant patients and those close to them.
TMS may become a preferred alternative for severe treatment resistant conditions, but right now it is a promising therapeutic tool with moderate effectiveness comparable to medications and psychotherapy. Treating depression and PTSD remains challenging, and typically involves a multifaceted treatment plan.
References
Drevets WC, Savits J, Trimble M. (2008). The Subgenual Anterior Cingulate Cortex in Mood Disorders. CNS Spectrums, Aug; 13(8): 663-681.
Philip NS, Barredo J, van 't Wout-Frank M, Tyrka AR, Price LH, and Carmpenter LL. (2018). Network mechanisms of clinical response to transcranial magnetic stimulation in posttraumatic stress disorder and major depressive disorder. Biological Psychiatry, Feb; 83: 263-272.




