Depression
Depression: A Deal With the Devil?
A genetic vulnerability to depression may protect you from infectious disease.
Posted August 31, 2012

Clinical depression is a problem that we know affects tens of millions of people in the United States alone every year. We know there is a genetic vulnerability to getting depressed, along with environmental contributors such as childhood trauma and recent stress. But why are humans vulnerable to depression? It doesn’t seem to be a very adaptive trait, after all. Hard to imagine a depressed hunter-gatherer making it for very long, raising children, collecting food.
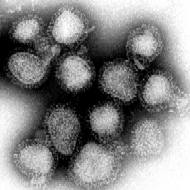
However, there may well be a genetic advantage that comes with the vulnerability to depression. It became important more so when humans began to live with animals in large groups, leading to the spread of infectious disease. But infectious disease has caused strong selection pressure on the human population in the recent millennia, so these genetic vulnerabilities could easily become widespread.
The paper I reference today is available full text online (from a Nature offshoot, Molecular Psychiatry) with the provocative name of PATHOS-D. It is really an amazing paper. If you are of a scientific bent, go over and take a peek.
Here is the theory. Depression*, as we know, is associated with certain types of inflammation in the brain. There are certain red immune system flags we see with the syndrome of depression quite frequently, most specifically increases in the cytokines TNF-alpha, IL-6, and C-reactive protein. These chemicals found in the blood and spinal fluid tell us a brigade of our immune system is on high alert, kicking a** and taking names, so to speak. Problem is, when there are no invading a**es left to kick (or the invaders are too clever and elude our defenses), our brains get the full onslaught and neurons die and then you can't concentrate, and you avoid social activities, and you may find yourself crying a lot, and your primary care doctor might recommend that you see a therapist or someone like me.
And we certainly know that genes in combination with stress will predispose us to depression. But some folks are bulletproof. They won't get depressed in the most dire of circumstances. Other people seem to be far more vulnerable. All it takes is a bit of a mismatch between temperament of parent and child and we have major psychopathology. A predisposition to depression is hereditary, therefore it must be encoded in our genes. But what genes? The PATHOS-D authors would suggest that the genes that predispose us to depression also protect us from infection.
Infection? All of us humans in the brave new modern world have endured 10,000 years of agriculture, which brought with it dense population and massive infectious disease. Tuberculosis, for example, is said to have killed most humans who have ever lived. The same genes that might give us a genetic advantage against infectious pathogens may lead to vulnerability to depression.
Inflammation, like an army, is a double-edged sword. People with trigger-happy immune systems are more likely to survive many infections (though a tricky beast like the 1919 flu killed the young adults with the most robust immune systems via massive pulmonary immune reactions and septic shock). Since infections in the developing world tend to preferentially kill young children, there is strong selection pressure for genes that will save you when you are young, even if those genes have a cost later in life. The selection pressure would have to be strong, as a clinical depression has obvious survival downsides, for both the person affected and his or her offspring. Depression tends to be chronically recurring and also will strike folks in 20s and 30s, unlike, say, Alzheimer's or most cardiovascular disease, thus selection pressure against depression alleles would likely be significant…unless those same alleles protected against something even more deadly that often strikes even younger, like infectious disease.
Cool theory, but where is the evidence?
Well, just as in schizophrenia, geneticists have tried to brute force hack the human genome in order to find a "depression gene." And just like in schizophrenia, they haven't had a lot of success. The answer (again, similar to schizophrenia and probably a lot of other diseases that don't fall into a simple single-gene model) will likely lie in looking at a group of genes for particular functions (say, immune function, or brain communication) and finding many different problems in those pathways in those who are genetically predisposed to depression. In all the genome searching, a couple of genes have come up consistently involved with depression in certain predisposed families. Both of them happen to be involved with cytokine signaling/immune function. That would be a heck of a coincidence.
One allele, -308A, was found to be associated with increased risk of depression along with decreased risk of tuberculosis infection, parvovirus B19, hepatitis B, and a lower risk of death when hospitalized while critically ill.
What about other genes that have been found to be associated with depression risk but weren't found on large population genome-wide association studies? We've discussed many of these genes and pathways in the history of this blog. MTHFR 677T is a version of methylenetetrahydrofolate reductase with reduced activity. That means the folate we eat in our diets will have a harder time being transformed into the folate that is active in the brain (methylfolate). Since folate is necessary to make things such as neuroransmitters and DNA, a brain without folate is in a sad state.
Low MTHFR is associated with increases in homocysteine and overall inflammatory tone. Since low folate is also associated with devastating birth defects, one would think there would be pretty strong selection pressure against this gene, but it is actually fairly common in the population. Why? Well, the inefficient version of MTHFR is found to be protective against cytomegalovirus infection, sexually transmitted disease, and hepatitis B. In places where there is sufficient folate in the food, MTHFR inefficiencies may not be too problematic and could mean protection against infections that cause other devastating birth defects and disease. In sub-Saharan Africa there is low folate availability, and the MTHFR 677T allele is nearly absent there.
ApoE is another molecule brain scientists find very interesting, primarily because different ApoE alleles confer different risks to certain diseases such as Alzheimer’s Dementia. ApoE is a signaling molecule located on the surface of lipoproteins (you might know of them as “good cholesterol” or “HDL” and “bad cholesterol” or “LDL,” which carry around fats and cholesterol and vitamins).
ApoE4 is the original, ancestral allele, and those who carry it have a higher risk for both Alzheimer's disease and depression. E4 is associated with increased inflammation in general. E2 is a protective version and means decreased risk of major depressive disorder and Alzheimer's compared to E4. The E4 allele may be protective against childhood diarrheal illnesses, while those with E2 seem to be more vulnerable to tuberculosis and malaria.
The most studied (and debated) alleles associated with depression are so-called short and long form of the 5HTTLPR. This gene is a promotor region that tells the cell to make a serotonin transporter. Those with the short allele (particularly with two short alleles) seem to have a much higher risk of developing major depression when exposed to early childhood trauma, whereas the long form of the gene is protective. However, the short gene isn't all bad. Those who have it seem to have a lower risk of dying from sudden infant death syndrome, and the gene is associated with higher circulating cytokines in response to stress, which could protect you if the stress is from being wounded or an infection. In populations where the short gene is more common, there also tends to be more exposure to epidemic infections, suggesting selection pressure for the short gene.
Finally, there is some thought put into the clinical syndrome of depression and how it might protect you and your offspring if you do have an acute infection. It is well known that inflammatory mediators (such as IL-6 or interferon) induce depression symptoms on their own. If you have come down with an infectious disease, being depressed would keep you isolated and conserve energy and reduce appetite. Interestingly, when you don't eat much for a little while, your body switches from burning glucose to burning another fuel called ketones. It is thought this process might improve immunity, as viruses and bacteria often love to burn glucose as well.
I think the strength of an evolutionary/ancestral paradigm for studying disease helps to provide a sensible framework, like the PATHOS-D theory. Clinically, it helps us to focus on the immune system and inflammation, and how that may have been altered by modern diet, stress, lack of parasites and pseudocommensals, changed sleep, infectious burden, and physical activity. Forget the random crapshoot of mere brute force epidemiology. There are too many confounders, and it will lead us in the wrong direction as often as not.
*here we are using the clinical definition of depression. Not just a sad mood for reason, such as grief. Usually we are talking about a sad mood with inability to enjoy things we used to enjoy, poor concentration, poor or unrestorative sleep, appetite change (classically poor appetite), guilt, self-doubt, and even suicidal thoughts.
Copyright Emily Deans, MD




