Caregiving
A Caregiver’s Guide to Tic Disorders
A quick guide to learn more about tic disorders and key resources.
Posted February 23, 2021
This post was written by Chelsea Dale, M.S.
Taylor’s mother noticed that her 8-year-old child was constantly sniffing but did not have a cold or allergies and was excessively blinking, head nodding, and making throat-clearing sounds for no apparent reason. When asked, Taylor described an inability to control the sounds and movements and a “funny” feeling in the neck that went away after nodding the head. What do all of these symptoms have in common? They may be the signs of a tic disorder.
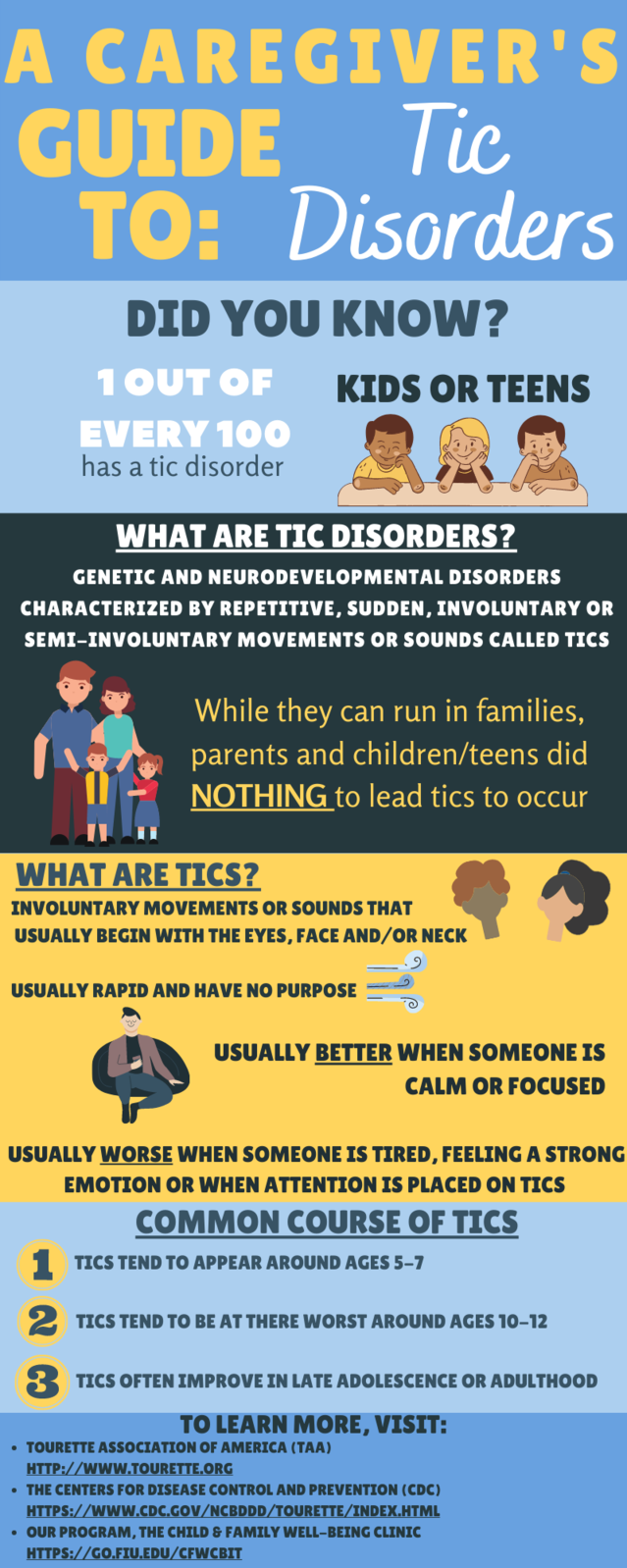
How common are tic disorders?
It is highly likely that a number of people that you know have had a tic disorder at some point in time. Transient tics (a tic or tics that appear but do not persist or cause distress or impairment) are common and impact up to 20% of school-age youth (Scahill et al., 2015).
Transient tics often disappear on their own. However, if they persist and prevent children from doing the things they like to do, it may be a good time to consult with a pediatrician or other medical or mental health professional (neurologist, psychologist, or psychiatrist). However, it is helpful to be familiar with certain signs and symptoms so you can feel prepared for the discussion.
What are tic disorders?
Motor tics involve body movements such as repeated shoulder shrugging, facial movements, or head jerking. Vocal or phonic tics include grunting, throat clearing, or making animal or bird sounds. These movements and sounds are involuntary (not done on purpose) and usually appear around age 6.
There are several types of tic disorders that differ mostly in how long the tics have existed, even if they have come and gone (waxed and waned) over this period of time. Tics occurring for less than a year are referred to as a provisional tic disorder. A chronic motor tic disorder involves only motor tics lasting for over one year; a chronic vocal tic disorder involves only vocal tics that have persisted for over one year. Tourette’s Disorder, often known as Tourette’s Syndrome, includes both motor and vocal tics which continue for over one year. While it is helpful to understand the differences, the treatments may be similar.
Can children with tics have other symptoms?
Many children with tics also have other symptoms. In fact, according to the CDC (Centers for Disease Control and Prevention, 2020), 86% of children diagnosed with Tourette's experience significant symptoms associated with another disorder. For example, 63% experience attention-deficit/hyperactivity disorder (ADHD) symptoms (hyperactive or impulsive and/or difficulty with attention or remaining on task), 49% experience anxiety (excessive worries or fears), and about 33% experience obsessive-compulsive disorder symptoms (unwanted thoughts that are reduced by doing certain behaviors — often referred to as rituals).
It is very common for tics to increase in intensity or frequency when children are tired, nervous, or very excited. Tics sometimes decrease when a child is feeling calmer and more relaxed. During your discussion with a medical or mental health provider, you may be asked about some of these other behaviors.
What happens when diagnosing a tic disorder?
When meeting with your provider, you will be asked questions about your child’s tics, such as what they look like, when they started, and how often they happen.
You may likely be referred to a neurologist to rule out other reasons that might better explain why your child is experiencing tics. Other diagnoses could include a seizure disorder or other neurological disorder, or another movement disorder. By evaluating these symptoms, your provider can determine the best course of treatment.
What do I do if my child is diagnosed with a tic disorder?
If your child is diagnosed with a tic disorder, there are some excellent and effective treatments to help you and your child manage their tics. If the tics are not upsetting the child and not interfering with activities they need to do or enjoy doing, it may not be necessary to seek treatment (however, communication with your provider is always important). For others, the tics may be problematic, and you may be referred to a practitioner familiar with appropriate treatment.
What kind of treatments are available?
The American Academy of Neurology (Pringsheim et al., 2019) recommends a behavioral intervention called Comprehensive Behavioral Intervention for Tics or CBIT as the first-choice treatment. CBIT involves learning skills and strategies in order to manage tics more successfully. You may also be taught strategies to help your child relax, such as taking deep breaths, which can reduce the frequency of tics. Learning new techniques can often help children and their families feel more confident in managing their child’s tics.
Some doctors may also suggest combining behavioral treatments, like CBIT, with medication; however, the evidence to support the effectiveness of these medications is mixed. Some doctors may prescribe a medication to help manage another disorder, like ADHD or anxiety. It is important to talk with your doctor about all treatment options and to determine the treatment that will be best for you and your family.
What causes tics?
It is important to remember that your child’s tics are involuntary and that no one did anything to cause them to occur.
What can I do as a parent?
You can try to limit the amount of attention focused on the tics. For example, instead of asking the child to stop, praise them for taking a calm and deep breath when they were feeling nervous. You might choose to take deep breaths along with your child. In fact, adults can also benefit from using strategies to help them calm down.
Important things to remember
Children with tics can be successful in whatever they choose to do. Tim Howard, a professional soccer player, Billie Eilish, a five-time Grammy award winner, and Dan Aykroyd, actor, producer, comedian, and filmmaker known for his time on Saturday Night Live and his starring role in The Blues Brothers and Ghostbusters all have been diagnosed with a tic disorder.
To learn more about tic disorders, find helpful resources, or locate a treatment provider, visit:
- Tourette Association of America’s website
- Centers for Disease Control and Prevention (CDC)’s website
You can also visit our university-based clinic’s website for more information about tics and to learn more about the free services we offer. Currently, our program offers services via telehealth.
Chelsea Dale, M.S., is a doctoral candidate in the clinical science Ph.D. program and a member of the Child and Family Well-Being Lab (CFW) at Florida International University.
References
Centers for Disease Control and Prevention. (2020, June 12). Data and Statistics on Tourette Syndrome. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/tourette/data.html.
Pringsheim, T., Okun, M. S., Muller-Vahl, K., Martino, D., Jankovic, J., Cavanna, A. E., Woods, D. W., Robinson, M., Jarvie, E., Roessner, V., Oskoui, M., Holler-Managan, H., & Piacentini, J. (2019). Practice guideline recommendations summary: Treatment of tics in people with Tourette syndrome and chronic tic disorders. Neurology, 92, 896-906
Scahill, L., Specht, M., Page, C. (2015). The prevalence of tic disorders and clinical characteristics in children. Journal of Obsessive-Compulsive and Related Disorders, 3(4), 394-400. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4243175/#:~:text=Transient….




