HiTOP Is a New Map of Mental Illness
A data-driven approach has produced a bold alternative model for diagnosis.
By Matt Huston published February 7, 2020 - last reviewed on March 20, 2020

Burdened by waves of anxiety, feelings of restlessness, difficulty sleeping, and fatigue, a woman we’ll call Jane makes an appointment with a local therapist. She reveals in her first session that she is also deeply uneasy about speaking to people she doesn’t know well and avoids doing so. Adding to her angst, she fears enclosed spaces and regularly refuses to take the elevator.
The clinician who meets Jane today will likely rely on the mental health profession’s go-to guidebook, the Diagnostic and Statistical Manual of Mental Disorders (DSM). In the U.S., it codifies behavioral health diagnoses, which fall into distinct categories such as generalized anxiety disorder, social anxiety disorder, and specific phobias.
Determining which categories best fit a person’s symptoms, however, is not always straightforward. “The typical patient in a psychiatric setting, if a thorough review of signs and symptoms is done, will meet criteria for more than one categorical disorder,” says Robert Krueger, a psychologist at the University of Minnesota who contributed to the latest edition of the diagnostic handbook, DSM-5. For some diagnostic labels, research suggests, different clinicians are liable to make different judgments about whether the label should apply.
About a hundred experts argue that there’s a better way.
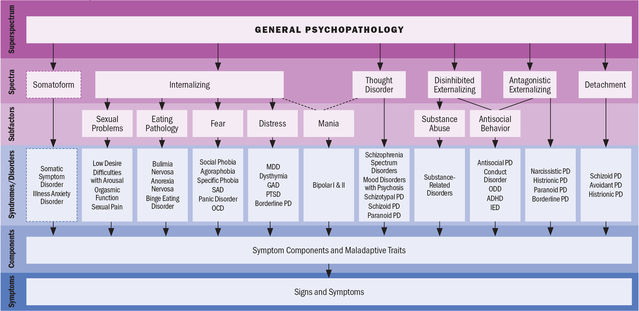
The model they have developed—called the Hierarchical Taxonomy of Psychopathology, or HiTOP—accounts for mental illness at multiple conceptual levels. It covers specific symptoms (such as avoidance, social anxiety, and suicidality) and traits (callousness, distractibility), but also more general factors with names such as Distress and Fear.
The model is dimensional: A person can score low, high, or somewhere in between on various measures. These severity scores can apply to the more general factors of psychopathology as well as to the narrower ones. As proponents of the model note, evidence suggests that most kinds of psychopathology lie on a continuum with normality.
Instead of diagnosing a person with one or more distinct disorders, the thinking goes, a therapist using HiTOP could identify a nuanced and holistic picture of a person’s mental illness—one that the developers hope will both reflect reality more accurately and enable more focused treatment.
In Jane’s (hypothetical) case, her anxieties and fear of elevators would be reflected in high scores on a general factor called “Internalizing,” a broad spectrum that includes forms of depression and anxiety. She’d also score highly on the Fear subfactor, and on certain underlying symptoms and traits.
Seeing a mental health professional schooled in the HiTOP model “would be like going to your physician,” says Christopher Hopwood, a clinical psychologist at the University of California, Davis and a member of the HiTOP consortium. “Physicians check your vascular system, nervous system, and other systems, and if there’s any evidence that something’s awry in your blood, let’s say, then they do more specific tests to try to home in on the dysfunction.” A clinician using HiTOP could evaluate a client using similar logic, he explains, screening first for signs of trouble in any high-level dimensions, such as Internalizing. When Jane scores highly on Internalizing, a clinician could probe for increasingly specific factors.

This top-to-bottom approach could help clinicians determine the best targets for treatment, Hopwood explains. “If a person is generally not depressed or anxious but has panic attacks, then the treatment ought to target that particular symptom like a laser,” he says. “But a lot of people are just general internalizers, so they’re going to have an array of issues that could be classified as panic, phobias, depression, generalized anxiety, OCD. And when that is the case, it probably makes sense to move up from those specific things and have a treatment that targets the general propensity to be internalizing.”
HiTOP’s approach will likely resonate with mental health care providers, Hopwood suggests: “I’ve never met a clinician who thinks that people come in [the DSM’s] diagnostic categories.”
A Bird's-Eye View
HiTOP, which was initially proposed in an article in the Journal of Abnormal Psychology in 2017, re-envisions the landscape of mental illness in large part based on the way that symptoms cluster together and how disorders, as currently defined, tend to co-occur. Broad, higher-level factors are based on analyses of these associations and of related data—such as those showing shared genetic vulnerabilities for different forms of mental illness. The highest-level proposed factor reflects the severity of psychopathology in general.
“We have a principled picture at the broad [upper] levels, spectra and subfactors,” says Stony Brook University clinical psychologist Roman Kotov, who is a HiTOP consortium founder along with Krueger and David Watson of the University of Notre Dame. A middle section in the model chart, for syndromes, currently lists traditional diagnostic categories such as major depressive disorder (MDD), but Kotov says that this is intended for communication purposes, “as we don’t yet have consensus on what HiTOP syndromes look like.” As the model is refined, parts of this level may differ substantially from the DSM’s descriptions.
A clinician using HiTOP could deploy an array of diagnostic measures to gain “a nuanced understanding of what kinds of symptoms a person is presenting with,” says Camilo Ruggero, a clinical psychologist at the University of North Texas who is involved in the project. The measures would yield a set of scores denoting how the patient compares to other people on broad dimensions, such as Thought Disorder or Detachment, as well as on narrower ones that include specific symptoms and traits. Reality distortion and inexpressiveness, would, for example, be associated with Thought Disorder, whereas intimacy avoidance and suspiciousness fall under Detachment.
What counts as a problematic set of scores in the realm of psychopathology is an unresolved question. In the DSM paradigm, if a patient meets a set of various criteria (“Two [or more] of the following, each present for a significant portion of time during a one-month period”), then he can receive a corresponding diagnosis. But HiTOP largely treats psychopathology in terms of continuous dimensions with no obvious, natural cutoffs. Multiple thresholds for clinical intervention could be one way around this. In future iterations of HiTOP, Ruggero says, “there might be one level of severity that simply requires surveillance, whereas another might require outpatient visits and another might require hospitalization.” Determining where to start drawing these lines will require more research—some of which, he reports, is underway.
James Potash, director of the Department of Psychiatry and Behavioral Sciences at Johns Hopkins Medicine, has some reservations about HiTOP—he argues, for instance, that a DSM-style cutoff can be useful for making dichotomous decisions, such as whether or not to prescribe medication. But Potash, who is not involved with the consortium, says that “aspects of what they’re trying to do could in some ways simplify and rationalize what the DSM does. Some patients generate many, many diagnostic categories,” a conundrum that HiTOP remedies by rejecting the category-centered approach. A therapy client like Jane can receive an overall dimensional profile—showing elevations on phobia and anxiety symptoms and on the broader factors that encompass them—in place of what could otherwise be several different DSM diagnoses.

HiTOP could also help address thorny questions about how certain forms of mental illness should be defined. Schizoaffective disorder, which the DSM describes as a combination of consistently disordered mood and delusions or hallucinations, “has been quite vexing in the DSM, because every version in the last 30 years has changed how it looks at the disorder,” says Potash. “It’s meant to be halfway between schizophrenia and mood disorder. How that in-between space should be delineated is something that people have had trouble agreeing on.” Rather than placing patients with a mix of psychotic and mood-related symptoms in this indistinct category, Kotov notes, HiTOP instead breaks down their experiences, in a granular way, along the continuums of Thought Disorder, Internalizing, and Detachment, “so the symptoms are characterized with high precision, and no arbitrary boundaries are needed.”
Work in Progress
The HiTOP consortium includes psychiatrists (and other nonpsychologists), but it arguably takes a relatively psychological approach to mental illness. Psychological research on personality, for example, treats personality traits as dimensional and “has involved using sophisticated methodologies to try to uncover the structure of personality,” notes psychologist Scott Lilienfeld at Emory University.
“The DSM has often been interpreted—in my view, misinterpreted—as implying that we have distinct disease entities that are either all or none,” says Lilienfeld, who is not part of the HiTOP consortium. “Developers of the DSM rejected that claim, but that’s been forgotten. HiTOP, I think, will remind people that what we’re talking about, in many cases, are variations on a dimension.”
Whether HiTOP will ultimately result in better treatment outcomes is an open question. While elements of HiTOP are “are widely used clinically and in research,” according to Kotov, clinical use of the full model has been limited. According to Ruggero, two field trials are underway to gather data about HiTOP’s feasibility and useability.
HiTOP has limitations. It relies heavily (though not entirely) on questionnaire and interview data from cross-sectional studies, which examine the relationships between measures of psychopathology at a single point in time. A critique of HiTOP in the journal World Psychiatry charged that it does not adequately capture how mental disorders develop over time. “It is true that the HiTOP consortium needs to further integrate aspects of illness trajectory and developmental influences into the model,” Kotov acknowledges. “We are working on this.” But HiTOP’s primary aim is to describe mental illness, not explain what causes it.
Some forms of psychopathology have not yet been integrated into HiTOP, and Kotov says that will require further studies. But ongoing revision is part of the plan. “It’s not necessarily going to be big editions like the DSM has gone through, but more incremental, specific changes that happen regularly, maybe multiple times a year,” Kotov says.
The dominant guidelines for diagnosis are not going away anytime soon. Clinicians currently use the DSM and its counterpart, the International Classification of Diseases (ICD), to get paid by insurers, so the consortium has created a guide for translating HiTOP assessments into analogous traditional diagnoses.
To a limited extent, however, the dimensional approach has already gained some traction. The model for personality disorders in the forthcoming edition of the ICD “is kind of a dimensional, trait-based approach to conceptualizing personality pathology,” Krueger notes. And Kotov points out that there are some dimensional aspects of the DSM-5, such as severity descriptors for substance use disorders and the autism spectrum.
Could those systems eventually move even further in HiTOP’s direction? “If official psychiatric nomenclature were to pick up elements of HiTOP, to assimilate it,” Kotov says, “that would be a success.”
LinkedIn Image Credit: Pormezz/Shutterstock
