Catching Madness
Can we catch OCD, anorexia, or schizophrenia the way we can the flu?
By Harriet Washington published November 3, 2015 - last reviewed on June 10, 2016
Cats have been viral on the internet for years. The fractured grammar of LOLcats "I can has cheezburger?" is as ubiquitous as the animal itself. As far as domesticated animals go, cats are an oddly appropriate meme because they carry viruses that the world is only now fully recognizing.
E. Fuller Torrey, a psychiatrist with the Stanley Medical Research Institute, has been studying the connection between cats, parasites, and mental illness. According to Torrey, a known parasite that can lead to madness is carried by the common household cat. In his book, The Invisible Plague, he reveals that around 1808, schizophrenia was swiftly transformed from a rare to a relatively common disease. That same year, as cat ownership became popular in the United States, as well as in other parts of the world, U.S. schizophrenia rates rose sharply.
This is no coincidence, Torrey contends. Cats transmit the one-celled parasite Toxoplasma gondii that causes the disease toxoplasmosis. It is already implicated in prenatal brain damage, abnormal head size, deafness, seizures, cerebral palsy, retinal damage, and mental retardation. Torrey and others think it does more: They argue that T. gondii infection causes schizophrenia.
Researchers are unmasking the microbial roots of myriad illnesses; maladies as seemingly trivial as a sore throat can breed anorexia, Tourette's, obsessive-compulsive disorder, or schizophrenia. Researchers estimate that infectious organisms cause from 10 percent to 75 percent of serious mental disorders. Bacteria, viruses, fungi, and other infectious agents are responsible for many of the illnesses that we have long ascribed to genetics.
As for T. gondii, Torrey and colleagues suspect that it causes subtle changes to an infected fetus that could lead to schizophrenia 20 years later. In 2008, Torrey and Robert Yolken of Johns Hopkins published a study indicating that the peak age for becoming infected by T. gondii, between 18 and 35, coincides with the peak age for the first signs of schizophrenia. They also noted that in areas where felines are rare the prevalence rates of both toxoplasmosis and schizophrenia are low. By 2005, studies reported in journals like the American Journal of Psychiatry found that children of mothers who contracted T. gondii while pregnant had higher rates of schizophrenia in adulthood than did other children. But Torrey also found that, in fact, the most strongly positive schizophrenia correlations were not with T. gondii infections acquired in the womb, but with those that struck children and teenagers.
Torrey and Yolken argue that sandboxes are a possible culprit. "A likely mechanism for exposure to T. gondii in childhood is playing in the dirt of sandboxes contaminated with T. gondii oocysts," they write, explaining that each uncovered public sandbox studied is used as a litterbox by four to 24 cats. The cats shed T. gondii eggs and cysts that find their way onto the hands of children. The sandboxes provide convenient sites for research showing how urban areas where cats have a high rate of infection become areas where children's later schizophrenia rates are similarly elevated.
Can You "Catch" OCD?
Susan Swedo, the chief of pediatrics and developmental neuroscience at the National Institute of Mental Health, has investigated Sydenham's chorea, a psychiatric disorder that can arise after exposure to a group A streptococcal, or GAS, infection, that results in symptoms such as a sore throat. Sydenham's, which mostly affects children ages 5 to 15, is characterized by rapid, involuntary, spasmodic movements, mostly of the face, feet, and hands. Chorea, from the Greek word for dance, refers to these movements, which are often accompanied by muscle weakness as well as emotional and behavioral problems.
Sydenham's is associated with rheumatic fever, which is caused by GAS that is untreated and is characterized by muscle aches, swollen and painful joints, skin rashes, and difficulty concentrating. As many as 30 percent of children who contract rheumatic fever develop Sydenham's. Although antibiotic use has rendered the fever rare in developed countries, it has recently made a comeback among the undertreated, such as inner-city children. Not only does Sydenham's follow streptococcal infections, but it is also seasonal, striking most frequently during the winter and early spring. In the U.S., it's most common in the northern states.
Because Sydenham's is in essence a rare complication of a strep infection, Swedo wondered whether such infections were associated with other psychiatric symptoms—like OCD. She suspected that the group A streptococcal, or GAS, infections that cause strep throat might also cause a brace of childhood mental disorders—OCD, Tourette's syndrome, anorexia, and other psychiatric conditions.
She knew that for some children, psychiatric symptoms are the first harbingers of Sydenham's: The children become unusually restless, aggressive, or hyperemotional even before the physical symptoms of chorea appear. They also display frequent mood changes, uncontrollable crying, and behavioral regression. Similarly, in the most common childhood psychiatric syndrome, OCD, intrusive thoughts or impulses recur, and children seem powerless to abandon their compulsive behaviors. Often, affected children are seized by fears of harm coming to a family member or of intruders. They sometimes feel compelled to count silently, wash their hands over and over, organize items, or repeatedly check whether the door has been locked.
Were the GAS infections really triggering mental disorders? "It was like a detective novel," Swedo recalls.
Swedo set about finding children who had also suddenly acquired OCD symptoms or tic disorders shortly after a bout with strep throat or other GAS infection. As word spread about her investigation, dozens of parents from the District of Columbia, Virginia, Maryland, and even as far away as Illinois and Michigan made pilgrimages to NIMH.
Swedo's team studied a group of 50 children with OCD, both with and without tics. All their symptoms had been preceded by strep throat or a similar infection. Tests found high levels of an antigen, a substance that stimulates an immune response against a pathogen, that suggested a genetic susceptibility to rheumatic fever and to Sydenham's chorea.
In 1998, Swedo published the landmark paper that laid out her theory of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections, or PANDAS, which appeared to afflict normally behaved children who fell into madness within days, sometimes overnight.
PANDAS is a syndrome, which means that it encompasses a number of disorders—OCD, Tourette's, anorexia, and others—that share a cause. Swedo and other scientists estimate that PANDAS accounts for perhaps three of every 20 cases of such conditions: She cautioned researchers that PANDAS was not a default diagnosis and should be considered only in cases where the conventional model of illness did not explain a child's symptoms.
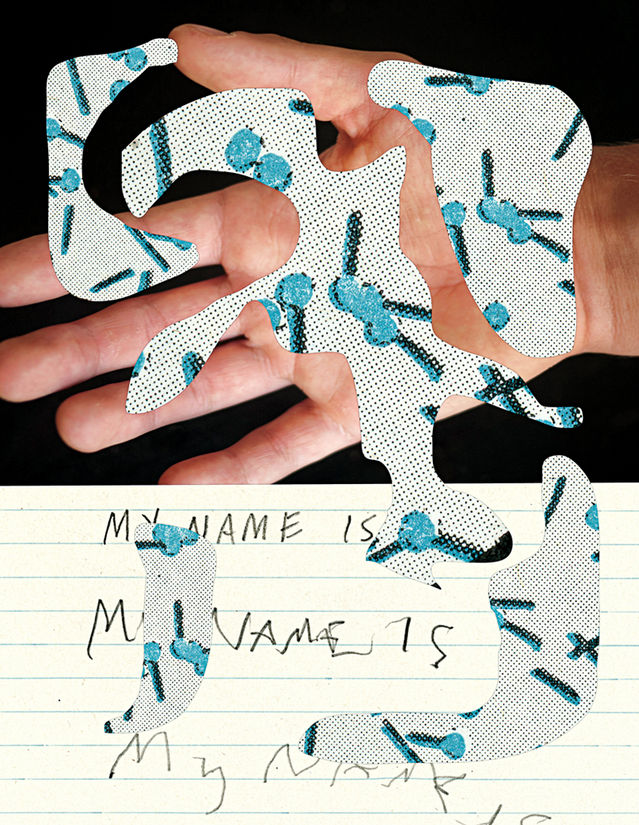
One of the most distinctive features is rapid onset; in the case of PANDAS, symptoms arise a few days after infection, while Sydenham's lag six to nine months after exposure. PANDAS symptoms show a gender disparity, with boys more likely to have tics and girls more likely to have obsessive compulsiveness. Moreover, PANDAS children regress in ways that other Sydenham's, OCD, and Tourette's patients do not. PANDAS children suffer a rapid deterioration of fine motor control as shown by the loss of handwriting and drawing skills, whereas the loss is more gradual in Sydenham's. A picture drawn by a 16-year-old PANDAS sufferer looks like the work of a 6-year-old. This instant infantilism extends to other behaviors. Preteens resume bed-wetting, and some find that they cannot stem the flow of their urine even during the daytime. They also begin to throw tantrums and refuse to speak and eat—though the latter is often triggered by an unshakable conviction that their food has been tainted or poisoned.
Unpacking Tourette's
Swedo found that the body's response to an infection can go haywire in a young person when an inexperienced immune system generates vigorous "friendly fire" that ends by damaging the body's own tissues instead of wiping out the invaders. In the model proposed by Swedo, the antibodies that normally fight infection and then subside linger long enough to interfere with the functioning of the brain's basal ganglia, which are involved in coordination of movement.
Because after an infection some children with PANDAS suffer from tics—including grunts, vocal utterances, and even curses—Swedo began to think they might suffer from a form of Tourette's syndrome as well.
About 200,000 Americans have the most severe form of Tourette's, a neurological disorder usually diagnosed in children between 3 and 9 years old and characterized by repetitive, involuntary movements and shouts, eye blinks, grunts, vocalizations, even barking, that are collectively called tics. Some experience more complex motor tics that include facial grimacing, head twists, and shoulder shrugs. Tics are often more severe during periods of excitement or anxiety. As many as one in every 100 Americans now show mild symptoms.
There are no blood, imaging, or lab tests for Tourette's; instead, diagnosis requires the presence of both motor and vocal tics for at least one year. Tourette's is chronic in 10 to 15 percent of affected people, but most children who are diagnosed weather the worst symptoms throughout their early teens; the tics gradually subside as they enter adulthood. This timing suggested a connection to PANDAS in Swedo's eyes, but more studies were necessary to prove the causal connection and to characterize the mechanism by which GAS causes mental disease. Swedo sought to discover whether giving treatment that fights GAS infections, such as filtering antibodies from the children's blood, would reliably alleviate the Tourette's symptoms.
As she recruited more children with GAS-related experiences, the word spread through pediatricians' offices, support groups, and mommy blogs, resonating with many parents who felt that an insidious infection, not genetics or family tension, was behind their children's OCD, anorexia, or Tourette's.
On one blog, a mother from Flint, Michigan, shared the story of her daughter Lisa*, who went to bed an "outgoing, friendly, and spunky" 9-year-old and "woke up transformed" into a toddler, erupting in screams, tantrums, and whining at the slightest frustration. Lisa reverted to bed-wetting and baby talk and seemed tortured by a compulsion to repeatedly touch surfaces and door handles, crying, "Mommy, Mommy, help me. I can't stop doing this!'' Even her handwriting and drawing reverted to that of a 3-year-old. "It was as though she was possessed," Lisa's mother wrote.
Lisa's overnight descent into illness seemed unnatural, and her mother was convinced that something physiological was afoot. While Lisa took medication and saw a behavioral therapist, her mother read about Swedo's studies. They drove to Maryland, where Lisa joined a study of 27 children with obsessive-compulsive disorder. The treatment involved filtering the offending antibodies from the children's blood. Swedo also used steroids, intravenous immunoglobulins, and plasma exchange to treat the underlying infections in carefully controlled clinical trials.
As with most of the study's subjects, Lisa's symptoms abated. She was able to resist the compulsions almost immediately; and as her antibody levels fell, her verbal expression and handwriting returned to an age-appropriate level. Within a month, her speech returned to normal and her bubbly demeanor resurfaced. Of the 18 children diagnosed with and treated for PANDAS, all but two improved.
This improvement is important because it helps bridge the gap between correlation and causation. The high antibodies to the infection are not merely associated with the mental-illness symptoms; as the antibodies are removed, the symptoms abate, which suggests a causal relationship between the madness and the antibodies, and therefore the infection.
Another PANDAS illness that strikes mostly girls is anorexia. OCD and anorexia are related not only by their compulsive symptoms, but also by the fact that neurotransmitters malfunction in both. What's more, as in OCD and Tourette's, some cases of childhood anorexia are triggered or dramatically worsened by a GAS infection. In 2000, Swedo reported in the Journal of Child and Adolescent Psychopharmacology that, when she tested four children who showed the clinical signs of PANDAS anorexia, the same antigens were elevated as in the other PANDAS disorders, indicating the telltale GAS infections.
A Contested Diagnosis
Some experts have expressed skepticism and questioned whether the connection is really causal, noting that the frequent sore throats characteristic of PANDAS cases are too common to constitute a distinguishing feature, especially because strep throat is never diagnosed in some children.
Is PANDAS really distinct from garden-variety Tourette's and OCD? Critics point out that the discovery of PANDAS was made from case-finding among sick children who fit the general profile rather than from forward-looking studies of large numbers of children selected at random, and some wonder whether this method creates an illusion of causality.

Some see the ubiquity of GAS infections as evidence against PANDAS: Strep throat and related infections are everywhere, but Tourette's and OCD are not. Does this mean that GAS infection is a cofactor, insufficient to cause disease on its own but exacerbating the damage from genetics, stress, trauma, or even poor parenting? Or is GAS just a near-ubiquitous, innocent bystander? To those convinced of PANDAS's disease status, it is clear that not everyone infected with GAS becomes mentally ill, because many factors affect vulnerability. Genetics, immunological vigor, general state of health, and perhaps environmental insults may all determine who develops PANDAS and who is able to avoid antibody damage.
But how do we determine whether the evidence that correlates infection with PANDAS rises to proof of causation? This question applies not only to PANDAS but to all the putative links between infection and mental states.
Basic standards for proof of infectious-disease causation were laid in 1883 by the German bacteriologists Robert Koch and Friedrich Loeffler, whose criteria are called Koch's postulates. A suspected pathogen can be said to cause a disease only when:
1) The germ is consistently associated with the disease.
2) It can be isolated from the sick person and cultured.
3) Inoculating an organism with the pathogen should cause symptoms of the disease to appear.
Critics have invoked Koch's postulates to question the etiology of PANDAS and other madness caused by infection. But there are known limitations to the postulates: Some microbes that cause disease fail to fulfill them. Mary Mallon, or "Typhoid Mary," carried the fever without suffering signs or symptoms herself. This carrier scenario is so common in infectious disease, especially in viral diseases such as polio, herpes simplex, and hepatitis C, that it invalidates Koch's first postulate.
Koch's second postulate rests on shaky ground because some disease-causing micro-organisms, such as prions—infectious proteins that many think responsible for Creutzfeldt-Jakob disease—cannot be grown in culture.
Koch himself knew that the third postulate was flawed: Ever since the establishment of germ theory, it's been known that not all organisms exposed to a pathogen will fall ill. Immunological resistance, genetics, and variations of general health can affect the outcome.
"Koch's postulates are obsolete," says Ian Lipkin, M.D., the director of the Center for Immunity and Infection at Columbia University. They "require that you grow something, put it in an animal model, and replicate disease. But there are agents that you can't cultivate in laboratories. You have infectious agents for which there is no animal model because you have to have a receptor for the virus," he explains. "Or, you have to be able to grow the bacterium: All these things are difficult. That's why we classify agents as possible, probable, and definitive evidence of disease."
Hard-to-Swallow Proofs
Yet we often ignore science even when we have the evidence; the acceptance of PANDAS may be like the acceptance of H. pylori. Take Australian physicians Robin Warren and Barry Marshall. In 1982 they proved that Helicobacter
pylori, a familiar bacterium living in our intestinal tract, accounts for 90 percent of stomach and duodenal ulcers, as well as other gastric diseases including stomach cancers. But if H. pylori was discovered to cause most ulcers in 1982, why did doctors continue to prescribe Tagamet and antacids until 1994? And why does the medical literature show that John Lykoudis, M.D., of Missolonghi, Greece, was curing ulcer patients with antibiotics as far back as 1958? A perusal of the NIH PubMed site for gastroenterology journals tracing ulcer treatment shows that during the century before Marshall and Warren's breakthrough, an infectious cause of ulcers had been "discovered" on at least 15 separate occasions—in 1892 in Italy, 1899 in Poland, the 1960s in Iran, among others.
Without scientific publication or rigorous testing, the infection theory of ulcers was consigned to the forgotten annals. Lykoudis's notebooks detail a life blighted by professional frustration until his death in 1980, just two years before Warren and Marshall validated his life's work.
The duo could prove the connection because they had access to tools unknown to Lykoudis, including the flexible fiber-optic endoscope developed in the late 1970s, which provided a safe technique to view the stomach and to collect specimens from the gastric mucosa of patients. Modern nutrient media and incubation techniques also allowed Warren and Marshall to grow the organisms in culture, as Koch dictates.
In 1985, having satisfied Koch's postulates, Warren and Marshall published their findings that H. pylori, not stress and spices, causes ulcers. But once again, the H. pylori hypothesis failed to change physicians' behavior. According to the Centers for Disease Control, most physicians knew of the H. pylori association, but half of primary care doctors did not test their ulcer patients for it; they kept doling out acid suppressors. Despite their superior tools and access to publication, Warren and Marshall were about to share Lykoudis's professional fate: studied indifference and obscurity.
In the end, it took showmanship to get the medical world's attention. To illustrate his claim, Murray drank a beaker of H. pylori in culture in 1984, and within days he was nauseous and vomiting. An endoscopy revealed both H. pylori and gastritis, which Murray was able to banish with antibiotics. The fading of his symptoms in two weeks demonstrated, for at least the 15th time, that a microbe causes gastric woes and that antibiotics can cure them.

The infectious cause of ulcers finally entered the medical canon when, in 1997, the CDC spearheaded a public-health campaign to spread the word that ulcers are a curable infection. In 2005 Marshall and Barry scored the ultimate validation: the Nobel Prize in Medicine or Physiology.
Harriet Washington is the author of many books, including Deadly Monopolies, the
National Book Critics Circle Award-winner Medical Apartheid, and Infectious Madness. She was an editor at USA Today and won fellowships at Harvard School of Public Health and Stanford University. She was also named a research fellow in medical ethics at Harvard.
From the book Infectious Madness by Harriet A. Washington. Copyright © 2015 by Harriet Washington. Reprinted by permission of Little, Brown and Company, New York, NY. All rights reserved.
Submit your response to this story to letters@psychologytoday.com. If you would like us to consider your letter for publication, please include your name, city, and state. Letters may be edited for length and clarity. For more stories like this one, subscribe to Psychology Today, where this piece originally appeared.
Facebook image: Kanstantsin Navitski/Shutterstock
