Eating Disorders
Brain Tumors Masquerading as Eating Disorders
Early signs of a brain tumor might look like an eating disorder.
Posted October 21, 2023 Reviewed by Ray Parker
Key points
- Brain tumors are abnormal cell masses in the brain.
- Brain tumors can cause eating disorder-like symptoms, such as weight loss and binge eating.
- To rule out a brain tumor, physicians should conduct neurological exams when diagnosing an eating disorder.
Imagine you are a physician, and your new patient is a 13-year-old girl who hasn't finished a meal in two months. Her parents are concerned about her eating behavior and her dramatic weight loss.
The patient mentions that she is depressed and has headaches and muscle weakness.
What would you diagnose her with, given this patient's signs and symptoms? If you said "an eating disorder," you might be correct.
This patient has common signs and symptoms of an eating disorder, including food restriction, dramatic weight loss, and depression.1-2 She is also in the population most vulnerable to developing an eating disorder. About half of adolescent girls engage in some type of disordered eating.1 Finally, malnutrition from an eating disorder could explain her muscle weakness and headaches.
Nonetheless, while it seems obvious that this patient has an eating disorder, physicians should consider other diagnoses before making this conclusion. This is because, in some cases, these signs and symptoms could indicate a brain tumor.
Brain Tumors
Brain tumors are abnormal cell masses classified as benign (i.e., slow growth and confined to one area) or malignant (i.e., quick growth across multiple areas). While only malignant tumors are cancerous, all brain tumors are dangerous. This is because brain tumors put pressure on the brain in ways that can permanently alter brain and body functions (e.g., memory or vision).
Roughly 1 million Americans have a brain tumor; over 70 percent of these tumors are benign.3 Anyone can develop a brain tumor, but these are most common in people over 40, except primary brain tumors. Primary brain tumors are tumors that start in the brain, and they are most common in children and young adults.
Typical signs of a brain tumor are headaches, muscle weakness, sensory and personality changes, seizures, nausea or vomiting, and memory loss.3 Early on, however, there may be no observable signs of a brain tumor, and, in some cases, signs and symptoms might resemble other conditions, such as an eating disorder.
Brain Tumors and Eating Disorder Symptoms
Because different parts of the brain regulate different bodily functions, tumor location determines a patient's signs and symptoms. Brain tumors in the hypothalamus, a brain region that regulates eating behaviors, appetite, metabolism, and hormones, are most often associated with eating disorder-like symptoms.4 Tumors in the brain's frontal lobes, brainstem, or pituitary gland can also cause eating disorder-like symptoms.

The most common eating disorder-like signs and symptoms caused by a brain tumor include, but are not limited to, weight loss or weight gain, hyperactivity, compulsive and ritualistic behavior, binge eating, body image concerns, compulsive exercising, depression, anxiety, and food preoccupations.4
How brain tumors cause eating disorder-like symptoms is complex and depends on tumor location. One study found that children and adolescents with craniopharyngioma, a rare tumor in the hypothalamus or pituitary area, have unusually high insulin resistance levels and low insulin sensitivity compared to individuals without this tumor.5 These changes in insulin regulation might explain why some of these patients binge eat. In other cases, patients with pituitary tumors might develop hyperthyroidism, which could speed up their metabolism, resulting in weight loss.6
Misdiagnosing Brain Tumors as Eating Disorders

A case study involving a 17-year-old girl illustrates how easy it is for medical professionals to mistake a brain tumor for an eating disorder.7
In this case, the patient was experiencing depression and low appetite, as well as headaches, anhedonia, occasional visual blackouts, muscle weakness, nausea, and nighttime incontinence for several months. Her daily meal consisted of a handful of grapes, prompting her family to take her to the doctor for an evaluation. Her doctor diagnosed her with an eating disorder and depression and prescribed her medications for these conditions. This diagnosis made sense to the doctor, given that the patient's symptoms developed after a breakup with her boyfriend.
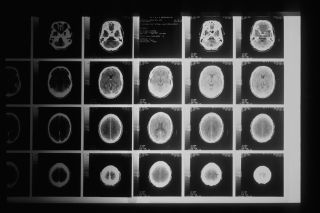
The patient's symptoms, however, worsened, and the frequency of her visual blackouts increased.7 Her parents brought her to the emergency room, where she received emergency care for her eating disorder. During this time, doctors noticed her pupils were heavily dilated and ordered a neurological examination followed by a brain imaging scan. The scan revealed a brain tumor.
After tumor removal, the patient's appetite fully returned, drastically improving her symptoms.7 Unfortunately, this isn't the only case where a brain tumor has been misdiagnosed as an eating disorder.8-10
What Should Physicians Do?
Brain tumors are challenging to diagnose and, therefore, are rarely diagnosed early in their development. The lack of early detection in brain tumor diagnoses is concerning because brain tumors can cause permanent damage to important bodily functions.

While eating disorders are more common than brain tumors, it is still important for medical professionals to rule out the possibility of a brain tumor when diagnosing a patient with an eating disorder. This is particularly important when a patient doesn't show typical signs of an eating disorder, such as body dissatisfaction, or has symptoms associated with brain tumors, such as vision difficulties.
When diagnosing patients with an eating disorder, physicians should perform tests for brain tumors, including a neurological exam to check coordination and balance and vision and hearing tests. If the results from these tests are concerning, specialists should conduct further tests. These extra steps might seem unnecessary, but they are vital for earlier brain tumor diagnoses and patient survival.
References
1.) Mallick N. Eating behaviors and body weight concerns among adolescent girls. Adv Public Health. 2014;2014. https://doi.org/10.1155/2014/257396.
2.) Godart NT, Perdereau F, Rein Z, et al. Comorbidity studies of eating disorders and mood disorders. Critical review of the literature. J Affect Disord. 2007;97:37-49. https://doi.org/10.1016/j.jad.2006.06.023.
3.) National Brain Tumor Society. Brain Tumor Facts. Braintumor.org. 2023. Retrieved from: https://braintumor.org/brain-tumors/about-brain-tumors/brain-tumor-fact….
4.) Uher R, Treasure J. Brain lesions and eating disorders. J Neurol Neurosurg Psychiatry. 2005;76:852-857. doi: 10.1136/jnnp.2004.048819.
5.) Roth CL, Gebhardt U, Müllet HL. Appetite-regulating hormone changes in patients with craniopharyngioma. Obes. 2011;19:36-42. doi:10.1038/oby.2010.80.
6.) Beck-Peccoz P, Persani L. TSH-induced hyperthyroidism caused by a pituitary tumor. Nature Clin Pract Endocrinol Metab. 2006;2:524-528. https://doi.org/10.1038/ncpendmet0276.
7.) Barnes A, Wang MM, Feltes J, et al. Subependymal giant-cell astrocytoma masquerading as restrictive eating disorder and depression in an adolescent. Innov Clin Neurosci. 2020;16:10-13.
8.) Niedzielska E, Węcławek-Tompol J, Kazanowska B, et al. Suspicion of anorexia nervosa as a cause of delayed diagnosis of brain tumor. A case report. Pediatr Endocrinol Diabetes Metab. 2015;20(3):123-128. doi: 10.18544/PEDM-20.03.0012.
9.) Distelmaier F, Janssen G, Mayatepek E, et al. Disseminate pilocytic astrocytoma involving brain stem and diencephalon: A history of atypical eating disorder and diagnostic delay. J Neurooncol. 2006;79:197-201. doi: 10.1007/s11060-006-9125-1.
10.) Houy E, Bebono B, Dechelotte P, et al. Anorexia nervosa associated with right frontal brain lesion. Int J Eat Disorder. 2007;40(8):758-761. https://doi.org/10.1002/eat.20439.
11.) O'Brien A, Hugo P, Stapleton S, et al. "Anorexia saved my life": Coincidental anorexia nervosa and cerebral meningioma. Int J Eat Disorder. 2001;30(3):346-349. https://doi.org/10.1002/eat.1095.




