Stress
The Surprising Link Between the Liver and Mental Health
... and why nearly half of American adults may be at risk.
Updated June 17, 2023 Reviewed by Tyler Woods
Key points
- Liver disease is a common but rarely recognized contributor to mental health symptoms.
- Non-alcoholic fatty liver disease is now the most prevalent liver condition, affecting a third of U.S. adults.
- A diseased liver can't protect the body or brain from toxins that cause physical and mental illness.
- Improvements in health and lifestyle habits are the best way to reverse early to moderate liver disease.
Julia thought she must be losing her mind. Ostensibly in her prime, at age 35, and working at a successful law firm, she began having panic attacks out of the blue at work. Her sleep deteriorated. She suffered from spells of brain fog and began making embarrassing mistakes at work. Finally, after finding herself on the side of the road after missing a turnoff she'd made 10,000 times before, she decided to speak with her physician.
Thankfully for Julia, the doctor didn't refer her to mental health. Instead, results from her metabolic tests revealed a more likely cause of her symptoms: advanced liver disease. In Julia's case, identifying and treating her liver disease not only reversed her mental health symptoms, it may have saved her life.
Right now, unfortunately, millions of Americans are experiencing some of the same symptoms as Julia, suffering from the same invisible process of liver pathology, but not understanding the connection or getting the right treatment.
The Liver and Mental Health
Anxiety, depression, mood swings, memory loss, sleep impairment, personality changes.
If the above symptoms make you think "mental illness," then you may be overlooking a potential cause now affecting nearly half of American adults: fatty liver disease. This once-rare condition results primarily from factors such as excess body fat, poor dietary practices, and alcohol and substance abuse.
Although most people know about obesity and diabetes, far fewer have heard about fatty liver disease, their close metabolic cousin. And almost no one realizes how closely their liver health is connected to their mental health.1 The aim of this post is to change that.
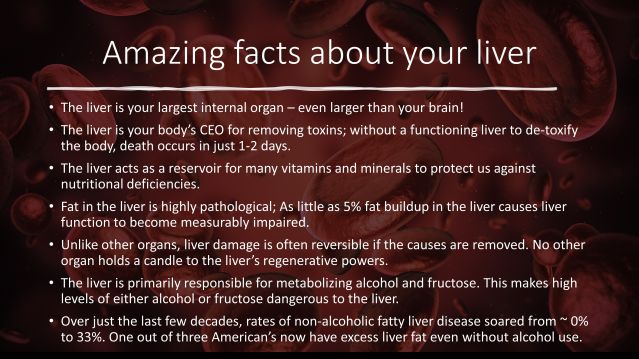
The liver is a remarkable organ, both for its staggering contributions to our overall health and for its vast underappreciation by the general public (see above figure). Outside of specialized liver doctors—such as hepatologists and gastroenterologists—even most healthcare providers do not realize the hundreds of life-enabling functions the liver performs each day.
The liver is the ultimate domestic engineer, working 24-7 to chemically neuter toxins in our blood before they infect our bodies. The organ functions as a nutritional warehouse for many essential vitamins and minerals and metabolizes medicines, alcohol, and other substances that would otherwise quickly jeopardize our existence.
The liver labors in these and many more roles in almost total obscurity, taking a relentless beating in the process of protecting us. Thankfully, the liver also just happens to be the organ equivalent of Wolverine—the fast-healing superhero mutant from the Marvel movies—in its ability to regenerate.
But even the marvelous liver has limits. Too much insulin, too much alcohol, or too much fructose, for example, and even the normally indomitable liver can no longer keep pace and begins to develop invasive fat within the liver tissue itself (the liver, under normal conditions, contains only trace amounts of fat).
The first signs of liver disease are sometimes recognized by physicians in the form of chronically elevated triglycerides, results on liver function tests such as alanine aminotransferase (ALT), or even by certain medical imaging procedures such as MRI and ultrasound. Caught early, fatty liver disease is treatable, frequently even reversible.
When these signs are missed, however, liver fat levels slowly progress, spiraling from the initial stages of inflammation to fibrosis and even cirrhosis. The latter cirrhosis stage is when the life-threatening process of liver failure ensues. As liver disease progresses across these stages, not only do many forms of physical illness become more likely, but symptoms of mental illness also increase.2

As shown in Figure 2 above, liver disease can be a direct cause of mental health symptoms because a compromised liver cannot prevent toxins in the blood from reaching the brain. These unwelcome invaders then proceed to wreak havoc on a range of critical brain functions. Concentration, memory, mood stability, and the ability to tolerate and respond to stress are just a few of the potential mental capacities that can be impaired when toxins begin accumulating in the brain. Sadly, fatty liver disease remains a silent epidemic in the U.S., with most people unaware of the signs, symptoms, or causes3.
Healthy Liver, Healthy Mind
Treating fatty liver disease is a good news/bad news situation. The bad news is that there are no medicines approved by the FDA for the treatment of fatty liver disease. Unlike high blood pressure, cholesterol, or glucose, there is no simple prescription drug for fatty liver disease.
Instead, the most effective treatments for improving fatty liver disease and liver-induced mental health symptoms are behavioral. Losing body fat—particularly abdominal area body fat—, reducing sugar and fructose intake, lowering insulin resistance through exercise, sleep, and stress management, and limiting or eliminating alcohol and certain medicines that can harm the liver in high quantities such as acetaminophen (Tylenol), are some of the best ways to improve liver function (particularly at early stages).
Because fatty liver disease is becoming more common each year in the U.S. population, a growing number of people will experience the physical and mental side effects of the condition. Talk to your doctor about liver function tests during healthcare visits, and remember how this much this vital organ contributes to your health and well-being.
Facebook image: Dragana Gordic/Shutterstock
LinkedIn image: F8 studio/Shutterstock
References
1. Labenz C, Huber Y, Michel M, et al.. Nonalcoholic fatty liver disease increases the risk of anxiety and depression. Hepatol Commun. 2020;4:1293–301.
2. Soto-Angona Ó, Anmella G, Valdés-Florido MJ, De Uribe-Viloria N, Carvalho AF, Penninx BWJH, Berk M. Non-alcoholic fatty liver disease (NAFLD) as a neglected metabolic companion of psychiatric disorders: common pathways and future approaches. BMC Med. 2020 Oct 1;18(1):261. doi: 10.1186/s12916-020-01713-8.
3. Ghevariya V, Sandar N, Patel K, Ghevariya N, Shah R, Aron J, Anand S. Knowing What's Out There: Awareness of Non-Alcoholic Fatty Liver Disease. Front Med (Lausanne). 2014 Mar 24;1:4. doi: 10.3389/fmed.2014.00004.




