Anxiety
The Turmoil of Uncertainty
Living with illness can create a state of suspended animation.
Posted March 27, 2023 Reviewed by Ekua Hagan
Key points
- Uncertainty is a subjective, cognitive state that can affect emotions and behavior.
- Research has tried to quantify the state of uncertainty but it's mainly qualitative, unlike risk and probability, which are statistical.
- Uncertainty is pervasive among patients and caregivers of those with medical illness but some have a higher tolerance for it than others.
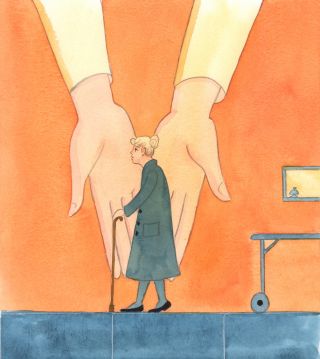
“When faced by uncertainty, we all oscillate wildly between panic and dismissal—as I was to discover when my cancer was first diagnosed,” writes English neurosurgeon Henry Marsh in And Finally: Matters of Life and Death (2022). Marsh continues, "One of the worst aspects of being a patient is waiting—waiting in drab outpatient areas, waiting for appointments, waiting for the results of tests and scans—living in a kind of 'suspended animation.'"
“Patients want certainty, but doctors can only deal in uncertainty,” writes Marsh. Only reluctantly could his physician quote him probabilities when Marsh learned of his prostate cancer and it became "increasingly difficult" to deny that his body "was past its Best Before date."
Researchers have attempted to develop scales to quantify uncertainty, but there are “no clear validated cut-offs” to define its levels. Fundamentally, then, uncertainty is a subjective cognitive state that may affect our emotions and behavior and involves vagueness, not knowing, and an inability to determine meaning or predict an outcome (Verduzco-Aguirre et al, 2021); Mishel, 1988.)
For some, the notion of uncertainty is “rooted in a paradox:” When we don’t have enough knowledge, the problem is that the future is different from the past whereas a solution, “depends on the future being like the past.’” In other words, says early 20th-century philosopher William James, "We live forward, we understand backward" (as quoted in Rizzo and Dold, 2021). Further, uncertainty is seen along a continuum so that “many of our real-world problems must be seen as mixed cases of risk and uncertainty” (Rizzo and Dold).
“The boundary between risk (i.e., statistical probability) and true uncertainty is not sharp and is a matter of degree:” probability, which is calculable, is simply “a degree of belief” (Faulkner et al, 2021.) Uncertainty is qualitative and involves situations where “people are unable or reluctant to assign numerically defined probabilities” (Faulkner et al.)
In the context of illness, uncertainty likely develops when symptoms are inconsistent in intensity, frequency, location, or duration, such as those that occur in diseases with remissions and recurrences (Mishel, 1988.)
Uncertainty can involve ambiguity about the state of an illness, complexity about its treatment, lack of information about a diagnosis, and unpredictability in its course (Mishel, 1988). Though "pervasive" (Guan et al, 2021) in patients with life-threatening illness, uncertainty remains "under-researched" (Etkind et al, 2017). In the limited research conducted, though, it has been associated with being a self-perceived burden to caretakers (Saji et al, 2023) and considerable psychological stress in patients (Guan et al.)
Those living with illness uncertainty have described it as "certainty within uncertainty," "cyclical uncertainty," or even "psychological whiplash" (Langmuir et al, 2023.) Others have emphasized a "deeply unsettled" lack of control, a "loss of future plans," and a "much less defined future" (Shilling et al, 2017.)
Some patients and their caregivers have a higher tolerance for uncertainty than others. Researchers, though, explain that there remain "imprecision and variation" in measuring and conceptualizing uncertainty tolerance (Strout et al, 2018). It may reflect a balance between negative responses (e.g., anxiety, distress, and avoidance) and positive ones (e.g. hope and information-seeking) (Verduzco-Aguirre et al; Strout et al).
Some patients may want to maintain uncertainty “since it facilitates hope” (Mishel, 1988.) But when the level of uncertainty expands, it can reach a "critical threshold" and create instability and a "lost sense of coherence" (Mishel 1990.)

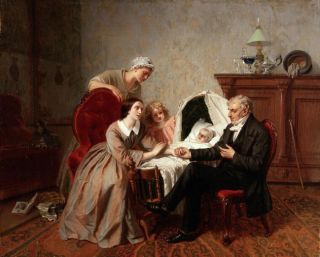
One area in which uncertainty can figure prominently is in issuing a prognosis, i.e., a prediction. Prognosis "gives diagnosis and therapy their affective components" for physicians and patients. It is essentially "the future of the present illness" (Christakis, 1999.) Even fifth-century B.C. Greek physician Hippocrates wrote a treatise on its importance in medicine. Prognosis can create a sense of meaning about the illness, but it may be both a source of uncertainty and a means of reassuring a patient and coping with uncertainty (Christakis.)
Physicians are often reluctant to make a prognosis because of fear of creating a self-fulfilling prophecy and because there is more uncertainty in predicting the future than in evaluating the present condition. Objectively, making a prognosis is difficult and potentially fraught with error that can have substantial consequences for a patient's care and a physician's reputation (Christakis). As a result, physicians may blur the distinction between an inability and an unwillingness to offer one.
They may also indulge in what Christakis refers to as "discrepant communication," i.e., communicating one prognosis to the patient and a different one to caregivers.
Further, physicians may see a "tension" between "population-based probability statistics" and their application to an individual patient (Christakis). Nevertheless, physicians will fall back on statistics, which Christakis refers to as "offering prognosis by the numbers."

The use of artificial intelligence (A.I.) in diagnosing, treating, and even offering a prognosis for an illness is increasing. Based on "big data," A.I. can extract hidden patterns and gather relevant information missed by a clinician (Liao et al, 2023.) Kahneman has described that algorithms are often superior to experts. For example, he reported a study that found major inconsistency among experienced radiologists, who contradicted themselves 20 percent of the time when they were shown the same X-ray at different times (2011.)
A.I., at least to date, though, has its challenges and limitations, including "disordered data" due to a lack of standards in the data used to build some models. Further, training sample sizes used to establish A.I. models are often small (Liao et al.) Eventually, though, A.I. may improve clinical judgment and patient care and may play a role in lessening medical uncertainty.
For a related topic, see my post, "Neither Sick Nor Healthy: Patients-in-Waiting."
References
Christakis NA. (1999). Death Foretold: Prophesy and Prognosis in Medical Care. Chicago: University of Chicago Press.
Etkind SN. (2017). How does uncertainty shape patient experience in advanced illness? A secondary analysis of qualitative data. Palliative Medicine 31(2): 171-180.
Faulkner P. et al (2021). F.H. Knight’s risk, uncertainty, and profit and J.M. Keynes’ Treatise on Probability after 100 years. Cambridge Journal of Economics 45: 857-882.
Guan T; Qan’ir Y; Song L. (2021). Systematic review of illness uncertainty management interventions for cancer patients and their family caregivers. Supportive Care in Cancer 29: 4623-4640.
Hippocrates. (1967). Prognostic, Volume II. T.E. Page et al, Editors. The Loeb Classical Library. Cambridge, Massachusetts: Harvard University Press. (English translation: W.H.S. Jones), pp. 1-55.
Kahneman D. (2011) Thinking Fast and Slow. New York: Farrar, Straus and Giroux.
Langmuir T. et al (2023). A new landscape in illness uncertainty: a systematic review and thematic synthesis of the experience of uncertainty in patients with advanced cancer receiving immunotherapy or targeted therapy. Psycho-Oncology 32: 356-367.
Liao J. et al (2023). Artificial Intelligence assists precision medicine in cancer treatment. Frontiers in Oncology 12: 998222 (16 pages.)
Marsh H. (2022) And Finally: Matters of Life and Death. New York: St. Martin’s Press.
Mishel MH. (1988). Uncertainty in illness. Image: Journal of Nursing Scholarship 20(4): 225-232.
Mishel MH (1990). Reconceptualization of the uncertainty in illness theory. Image: Journal of Nursing Scholarship 22(4): 256-262.
Rizzo MJ; Dold M. (2021). Knightian uncertainty: through a Jamesian window. Cambridge Journal of Economics 45: 967-988. (The authors quote philosopher-economist Frank Knight and philosopher William James.)
Saji A et al. (2023): Self-perceived burden for people with life-threatening illness: a qualitative systematic review. Journal of Pain and Symptom Management 65(3): e207-e217.
Shilling V. et al (2017). The pervasive nature of uncertainty-a qualitative study of patients with advanced cancer and their informal caregivers. Journal of Cancer Survivorship 11: 590-603.
Strout TD et al. (2018). Tolerance of uncertainty: a systematic review of health and healthcare-related outcomes. Patient Education and Counseling 101: 1518-1537.
Verduzco-Aguirre HC et al. (2021). Associations of uncertainty with psychological health and quality of life in older adults with advanced cancer. Journal of Pain and Symptom Management 61(2): 369-376.




