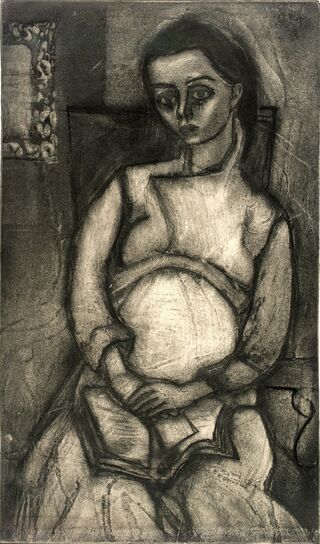
Pregnancy
Treating the Pregnant Woman with Pernicious Vomiting
Evolution in our thinking about symptoms during pregnancy.
Posted July 7, 2021 Reviewed by Vanessa Lancaster
Key points
- Years ago, physicians thought pernicious vomiting in pregnancy was psychological and imposed harsh and cruel behavioral methods on women.
- The cause of pernicious vomiting is still unknown but researchers believe there is a strong genetic component and implicate the hormone GDF15.
- Intractable symptoms can be severe, occur in each subsequent pregnancy, and require hospitalization for dehydration and electrolye imbalances.

“Having gotten the patient into the hospital, the vomit bowl is kept away from her. If she wants to vomit, she is told to vomit into the bed, and when she does vomit, the nurse is instructed not to be in too great a hurry to change her…I find that a certain curtness of manner works to advantage,” wrote an obstetrician in the 1920s (Atlee, 1925). He suggested to one patient that, if she needed to vomit, she should do so on a “particularly fine rug—a wedding present” she had brought to the hospital.
By today’s standards of care, this harsh behavioral conditioning, which may have worked for some, seems cruel treatment for pregnant women suffering from pernicious vomiting, i.e., hyperemesis gravidarum (HG), a disorder affecting up to 3% of pregnant women (London, 2017).
There is no consensus definition for HG nor even a complete understanding of its pathogenesis. The distinction between moderate and severe symptoms can be challenging (Fejzo et al., 2019) and often rests on clinical judgment (London et al., 2017). Physicians can assess the severity of vomiting by its frequency and duration with the validated Pregnancy-Unique Quantification of Emesis (PUQE) scale.
Importantly, when a pregnant woman presents with severe nausea and vomiting, particularly in the second trimester, clinicians must consider other diagnoses, including gastrointestinal (e.g., intestinal obstruction, hepatitis, appendicitis), genitourinary (e.g., kidney stones, pyelonephritis), metabolic (e.g., diabetic ketoacidosis, Addison’s disease, hyperthyroidism), neurological (e.g., migraine headaches, CNS tumors), other pregnancy-related (e.g., preeclampsia), and even miscellaneous (e.g., psychological, drug toxicity) conditions.
HG, in the absence of other diseases, becomes a diagnosis of exclusion. Typically, patients have severe dehydration, electrolyte imbalance (Petry et al., 2018), and a loss of 5% of their pre-pregnancy weight (London et al., 2017).
Hyperemesis gravidarum has been called a “disease of theories”(Kemp, 1933). Over the years, physicians have speculated that toxic metabolites cause it in a patient’s blood, abnormalities of pelvic organs (Stevens, 1905), or even adrenal insufficiency (Kemp, 1933). One early 20th-century theory held that HG was purely psychological, caused by hysteria or specific neurotic conflicts (e.g., ambivalence about being pregnant), a belief damaging to some patients. It led to minimizing their distress and mistreating them with aversive techniques (Munch, 2002).

Investigators have also considered infectious origins (e.g., H. pylori). Recently, elevated hormone levels of GDF15 are implicated, as are genetics, since women with a family history are three times more likely to experience HG (Petry et al., 2018). Increased GDF15 levels may suppress pro-inflammatory cytokines, facilitating the development of the placenta and maintaining the pregnancy (Fejzo et al., 2018).
Treatment for nausea and vomiting of pregnancy depends on the severity of symptoms. For mild symptoms, lifestyle modifications in diet (e.g., dry crackers, avoid spicy foods, eat small, frequent meals) or non-pharmacological remedies (e.g., massage, acupuncture) may help. Ginger has benefits, but there is no standardization of dose as with any plant or herbal preparation. Cannabis has been used for its anti-emetic properties, but the American College of Obstetricians and Gynecologists recommends against it. Though the mechanism is unknown, administering a multivitamin B complex at the time of conception (in those women who have planned their pregnancy) may decrease symptoms (Fejzo et al., 2019).

For more serious, intractable symptoms, clinicians must first assess the need for hospitalization. Recently, the media reported that Kate Middleton, Duchess of Cambridge, suffered from hyperemesis gravidarum during all three of her pregnancies (not uncommon), severe enough to require hospitalization. Before accurate methods to diagnose pregnancy and before intravenous hydration, women did die from HG. See my previous blog for a discussion of the speculation that 19th-century novelist Charlotte Brontë died due to hyperemesis gravidarum.
Medications are available, but only nine drugs have been approved officially for use in pregnancy. Only one for nausea and vomiting not responding to lifestyle changes: Diclegis, an extended-release combination of an antihistamine and the B6 vitamin pyridoxine (Wesley et al., 2021). Many other medications are used “off-label.” Between 40% to 60% of pregnant women reportedly take one or more prescription medications for either pre-existing conditions (e.g., diabetes, asthma) or pregnancy-related conditions (Ren et al., 2021).

In 2014, the Pregnancy and Lactation Labeling Rule eliminated the previous drug classifications ABCDX. The label now contains a risk summary of available evidence for use during pregnancy. However, clinical interpretation is still required, and in most cases, safety and dosing information is not available or “embarrassing scant” (Caritis and Venkataramanan, 2021).
Many physicians understandably remain reluctant to prescribe, and their pregnant patients reluctant to take, medications during pregnancy, particularly in the wake of the thalidomide tragedy of the early 1960s. It took five years for clinicians to connect thalidomide and the severe congenital disabilities, including the shortened, flipper-like limbs of phocomelia, that resulted. At least 10,000 babies were affected worldwide.

FDA advisor Frances Kelsey, M.D., Ph.D., resisted considerable pressure to approve the drug for use in the U.S. (Loughlin, 2017), even though it had been marketed to treat nausea and vomiting in pregnancy in 49 countries. Even a single 50 mg tablet during a “time-sensitive window" led to congenital disabilities is up to 50% of pregnancies (Vargesson, 2015).
This tragedy changed the entire drug-approval process: no longer could animal testing alone be sufficient (London Science Museum, 2019).
Investigators emphasize that pregnant women be protected by research rather than from research (Ren et al., 2021). However, clinicians are right to ask, “What level of evidence is required before exposing the first pregnant woman?” (Bahmanyar et al., 2021). Unfortunately, we don't always have the answer.
References
16 references follow in alphabetical order:
Atlee HB. (1925). The treatment of the pernicious vomiting of pregnancy. The Canadian Medical Association Journal. 15(4) 388-389.
Bahmanyar et al. (2021). Women and babies are dying from inertia: a collaborative framework for obstetrical drug development is urgently needed. American Journal of Obstetrics & Gynecology 225(1): 43-50.
Caritis SN, Venkataramanan R.(2021) Obstetrical, fetal, and lactation pharmacology—a crisis that can no longer be ignored. American Journal of Obstetrics & Gynecology 225(1): 10-20.
Committee on Obstetric Practice (2018). Clinical Management Guidelines for Obstetrician-Gynecologists. Obstetrics & Gynecology 131 (1), e15-e29.
Fejzo MS et al. (2018). Placenta and appetite genes GDF15 and IGFBP7 are associated with hyperemesis gravidarum. Nature Communications 9(1178): 1-9.
Fejzo MS et al. (2019). Nausea and vomiting of pregnancy and hyperemesis gravidarum. Nature Reviews 5(62): 1-17.
Kemp WN. (1933). Hyperemesis gravidarum treated as a temporary adrenal cortex insufficiency. The Canadian Medical Association Journal 28(4): 389-391.
London V et al. (2017). Hyperemesis Gravidarum: a review of recent literature. Pharmacology 100: 161-171.
Loughlin K. (2017) Frances Oldham Kelsey: a medical profile in courage. Hektoen International 9(3): https://hekint.org/2017/03/24/frances-oldham-kelsey-a-medical-profile-i…. (Retrieved 7/4/21).
Munch S. (2002). Chicken or the egg? The biological-psychological controversy surrounding hyperemesis gravidarum. Social Science & Medicine 55: 1267-1278.
Petry et al. (2018). Associations of vomiting and antiemetic use in pregnancy with levels of circulating GDF15 early in the second trimester: a nested case-control study. Wellcome Open Research 3(123): 1-14.
Ren Z et al (2021). Drug development research in pregnant and lactating women. American Journal of Obstetrics & Gynecology 225(1): 33-42.
Science Museum, London (11 December 2019): Thalidomide. https://www.sciencemuseum.org.uk/objects-and-stories/medicine/thalidomi… (Retrieved 7/3/21).
Stevens TG.(1905) Hyperemesis Gravidarum. Journal of Obstetrics and Gynaecology of the British Empire 7:266-75.
Vargesson N. (2015). Review: Thalidomide-induced teratogenesis: history and mechanisms. Birth Defects Research (Part C)105: 140-156.
Wesley BD et al. (2021). Prescription medications for use in pregnancy—perspective from the US Food and Drug Administration. American Journal of Obstetrics & Gynecology 225(1): 21-32.




