Neuroscience
Schizophrenia: Why Cerebellar-Cerebral Connectivity Matters
How the cerebellum and cerebral cortex connect affects schizophrenia symptoms.
Posted January 28, 2021 Reviewed by Matt Huston
"We don't know exactly what the cerebellum is doing; but whatever it's doing, it's doing a lot of it." —Richard Bergland, M.D., 20th-century neurosurgeon, neuroscientist, and author of The Fabric of Mind
Blogger's note: Before diving into the latest study (Cai et al., 2021) on schizophrenia and altered cerebellar-cerebral functional connectivity, I'm going to share some background information that puts this research in a personal and historical context.
When my late father, Richard Bergland (1932-2007), was training to be a neurosurgeon in the 1960s, all of the medical school textbooks described the cerebellum as a motor-function-only brain region that had nothing to do with cognition or neuropsychiatric disorders.
It wasn't until the very end of the 20th century (1998) when Jeremy Schmahmann and colleagues at Harvard Medical School published two seminal papers about "dysmetria of thought" and "cerebellar cognitive affective syndrome" (Schmahmann's syndrome) that non-motor functions of the cerebellum were put forth in peer-reviewed literature.
Throughout his career, my father had innumerable face-to-face encounters with neurosurgery patients who were experiencing cerebellar deficits or damage. Based on bedside observations and patient evaluations, Dad speculated that the cerebellum affected cerebral functions in ways that went beyond coordinating muscle movements.
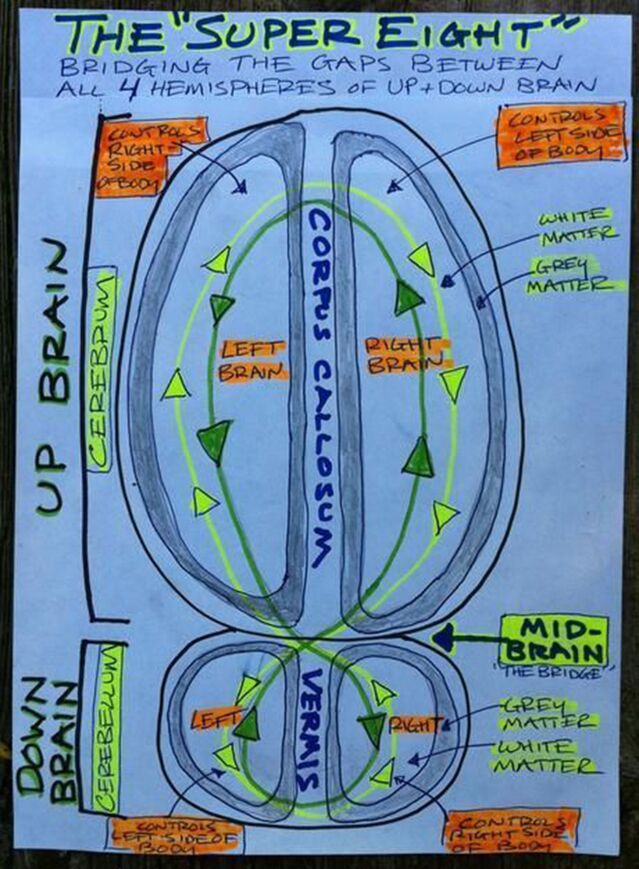
When I was a young tennis player in the 1970s, my father coached me to "beef up my cerebellum" through practice, practice, practice so that I wouldn't have to overthink by relying too much on my prefrontal cortex. Together, Dad and I created a split-brain model we called "up brain-down brain," which was the foundation of my first book The Athlete's Way (2007).
My father died unexpectedly a few months after The Athlete's Way was published. At his funeral, I made a commitment to keep my antennae up for new research that would help answer his lifelong quest to understand "what the cerebellum is doing."
Around 2009, I realized that the functional connectivity between regions within both hemispheres of the cerebral cortex and both cerebellar hemispheres is key. At the time, I drew a rudimentary "Super 8" brain map (below) using Sharpies and different colored highlighters to illustrate the importance of optimizing functional connectivity between the cerebellum and cerebrum. (See "Cerebro-Cerebellar Circuits Remind Us: To Know Is Not Enough.")
In the decade since I hastily sketched this brain map, I've been on the lookout for empirical evidence that would advance our understanding of how the cerebellum works and why cerebellar-cerebral functional connectivity matters.
This week, a new paper, "Neurological Soft Signs Are Associated With Altered Cerebellar-Cerebral Functional Connectivity in Schizophrenia," provides some new clues. This paper (Cai et al., 2021) was published on January 22 in Schizophrenia Bulletin.
Neurological soft signs (NSS) include deficits related to sensory integration, disinhibition, motor coordination, and the sequencing of complex motor skills. Previous research has shown that these "soft signs" are biomarkers for schizophrenia (SCZ) and suggests that the cerebellum plays a pivotal role in some of the cognitive and perceptual impairments observed in SCZ patients. (Chan et al., 2010)
However, until recently, relatively little has been known about how the sensory integration deficits observed in patients with schizophrenia may be linked to cerebellar-cerebral functional connectivity.
Recent research by Raymond Chan and colleagues at the Chinese Academy of Sciences's Institute of Psychology suggests that less robust cerebellum activity (i.e., cerebellar hypoactivation) is associated with sensory integration deficits in SCZ patients. "Importantly, the cerebellar activation underlying sensory integration is heritable," the authors explain in a January 26 news release. Chan is a researcher and professor of applied cognitive neuroscience and neuropsychology.
In their latest study, Chan's team, led by first author Xin-Lu Cai, focused on the "specific relationship of NSS and cerebellar-cerebral resting-state functional connectivity (rsFC) in 51 patients with schizophrenia and 50 healthy controls."
Their findings show that "cerebellar-prefrontal rsFC was positively correlated with negative symptoms in schizophrenia patients." They also identified "positive correlations between NSS and rsFC of the cerebellum with the inferior frontal gyrus and the precuneus, and negative correlations between NSS and rsFC of the cerebellum with the inferior temporal gyrus."
"These findings demonstrate the important role of cerebellum and its connection to cerebral cortex contributing to both the NSS manifestations and negative symptoms in patients with schizophrenia," Chan said in the news release. "Such altered cerebellar-cerebral functional connectivity may share the same neural mechanism for NSS and negative symptoms in this clinical group."
"Our results suggest that the uncoupling of resting state functional connectivity between the cerebellum and the cerebral cortex may underlie the expression of neurological soft signs in schizophrenia," the authors write in the paper's abstract. Based on these findings, Cai et al. conclude: "NSS-related cerebellar-prefrontal resting state functional connectivity may be a potential neural pathway for possible neural modulation to alleviate negative [SCZ] symptoms."
References
Xin-Lu Cai, Yong-Ming Wang, Yi Wang, Han-Yu Zhou, Jia Huang, Ya Wang, Simon S. Y. Lui, Arne Møller, Karen S. Y. Hung, Henry K. F. Mak, Pak C. Sham, Eric F. C. Cheung, Raymond C. K. Chan. "Neurological Soft Signs Are Associated With Altered Cerebellar-Cerebral Functional Connectivity in Schizophrenia." Schizophrenia Bulletin (First published: January 22, 2021) DOI: 10.1093/schbul/sbaa200
Raymond C. K. Chan, Ting Xu, R. Walter Heinrichs, Yue Yu, Ya Wang. "Neurological Soft Signs in Schizophrenia: A Meta-analysis." Schizophrenia Bulletin (First published: April 17, 2009) DOI: 10.1093/schbul/sbp011




