Alcoholism
Be a Well-Informed, Active Self-Manager of Your Medical Care
It could save your life.
Posted October 22, 2020
This is a guest post by Dr. Richard Contrada. As usual with guest posts, it is being presented here because I think it is interesting, and the views may or may not correspond to my own. I do think this one is particularly informative.
Although I am a health psychologist, I have probably learned less about dealing with medical problems in that role than I have through my experience as a chronic lymphocytic leukemia (CLL) patient. I have also benefited from using logic, critical thinking, and common sense, multipurpose tools at everyone’s disposal.
Before I share some of what I have learned, in the hope it may be of some use to others with chronic medical conditions that do not have simple and effective treatments, be warned: I am not a physician. Nothing I say can directly inform your diagnosis or treatment. But I can suggest ways to acquire, evaluate, and benefit from medical expertise.
My overarching recommendation is to be an active agent in managing your health care. Physicians work for you as expert consultants. But you must take charge of seeking out the best consultants, questioning and verifying what they say, and monitoring and interpreting diagnostic tests and therapeutic recommendations.
The following episodes all occurred while I was in the care of qualified providers at reputable medical institutions. There are some that many of you may find disturbing.
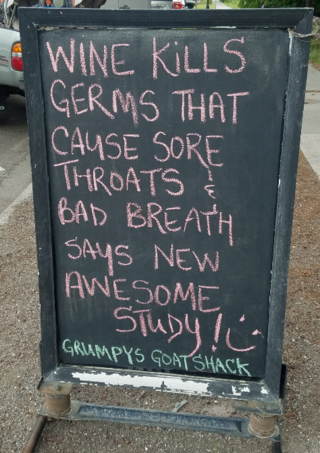
Have Some Pretzels With That Drink
Doctors are experts, but you know a few things too. In addressing my concern about growing fatigue, an oncologist at an internationally renowned cancer center suggested it may have developed because I recently reduced my alcohol intake and that I might want to reconsider that decision. At the time, I had been diagnosed with CLL, but was not yet being treated (a stage known as “WW” for “Watch and Wait” that feels more like “Wait and Worry”).
Problem is, alcohol is a central nervous system depressant.
Now, physicians receive much more training in diagnosis and treatment than in health-related lifestyle behaviors. But, surely, the oncologist knew this about alcohol. So why the recommendation? I have no idea. I knew that, at first, alcohol has stimulating and pleasurable subjective effects, but these are short-lived, whereas my fatigue had become chronic. Alcohol would not likely have helped, so I did not follow the suggestion. My guess: It was a kind of a placebo prescription, intended mainly to reduce my concerns.
Was the advice dangerous? Was something going on that required attention? Growing fatigue might have reflected increased systemic inflammation caused by the progression of CLL, which can produce “sickness behavior” symptoms that include fatigue. Perhaps additional testing would have identified this. What I do know is that the fatigue was followed by deterioration in my condition and hospitalization.
You know yourself. I once expressed to a nephrologist (kidney specialist) my concern about occasional orthostatic hypotension—lightheadedness caused by a blood pressure drop on rising from a seated position. It could have been a medication side effect since at this point my CLL was being treated. The kidneys regulate blood pressure in part by maintaining adequate blood volume via fluid retention. This is also facilitated by salt intake. The nephrologist advised me to eat pretzels.
I went with it. Why? I knew my blood pressure was generally low. I probably wasn’t drinking enough water, but was drinking caffeine- and alcohol-containing beverages, both of which reduce fluid retention. I also knew I could prevent the main danger—a fall—by taking a few deep breaths before standing and rising slowly. The upshot? I have made pretzels a regular part of my diet. And while not specifically recommended by the nephrologist, I began drinking more water, which fit with his “diagnosis”. The episodes stopped. Cause and effect? Who knows? But the pretzels do not seem to have caused any harm, and I have not needed any medication for the orthostatic hypotension that might have had side effects.
Lessons? This isn’t about alcohol and salt. It’s about something we all should do: Weigh the pros and cons before making important decisions, including medical decisions. Pretzels weren’t going to hurt; the recommendation fit with my low blood pressure and pattern of fluid consumption, and I could protect myself from falling.
However, developing a new symptom while in WW mode for a potentially deadly blood cancer probably warranted more scrutiny. When I eventually told the oncologist I was interested in a second opinion on whether, when, and how to treat the CLL, she called this “doctor shopping." So instead I engaged in “doctor switching.”
Another principle is that experimenting on yourself can be informative and useful if done carefully. The “carefully” part can’t be overstated. I would not play around with things like the dose levels of prescription drugs, or herbal “remedies” not evaluated for safety. But diet, exercise, sleep, and other aspects of lifestyle may be worth reviewing with your physician and modifying if not contraindicated.

On Blood and Other Fluids
The 4-day rule holds, but not the 3-second rule. While hospitalized for a serious infection, an IV clearly labeled for removal in four days was left in place. I did nothing about this, and on the fifth day, it infiltrated my arm which blew up like a balloon. During a different hospitalization, a phlebotomist picked up a syringe he dropped on the floor and prepared to draw blood. I told him I wanted a new phlebotomist.
Lessons? The failed IV was a rookie mistake. It occurred early in my patient career. I became a bit concerned on day 5, but concluded the IV was working properly, so why endure another needle stick? I don’t know if exceeding four days was intentional but I do know nurses and phlebotomists will bend rules. One thing I’ve seen is where they cut off the tip of one finger of their latex glove to get a better feel to locate a good vein. One expired IV and one “modified” glove were enough for me; well, those and a case of sepsis (a bacterial infection in your bloodstream) that nearly killed me. It was sepsis I had been hospitalized for when the phlebotomist tried to use the dropped syringe. I am now quicker to direct my bloodwork than I am to send a poorly prepared meal back to the kitchen. Be alert to outright incompetence; it’s your well-being, maybe even your life, which is at stake. And be assertive; in hospitals as well as in restaurants.
Never Mix/Never Worry Applies to Medication
The Internet can be your friend as well as your enemy. I was once hospitalized for a calcium level spike. Googling the possible implications was distressing. Nothing good comes from elevated calcium and there are horrific possibilities. I was prescribed three medications: one to treat CLL, the possible cause; an antacid to protect the lining of my stomach from steroids I was receiving but that also interfered with the absorption of the first drug, and a third medication that—wait for it—increased calcium levels.
Lessons? Humans are fallible, and so are the systems we create. What’s most relevant here is how the errors were detected: I started to Google my medications instead of my condition. By now a veteran of 7 hospitalizations in 10 years, I was beyond skeptical of medical interventions; my posture was frankly adversarial. I questioned every change in treatment, whether something was added or removed. I fought pain, bad food, and sleep deprivation to study my chart, and search the Internet to understand technical terms, and I discussed my symptoms, test results, and treatments with My Sister, The Nurse.
In this case, it was easy to find using an online medications site with a drug interaction tool showing that this particular drug would raise my already high calcium levels. It was just as easy to learn the antacid could interfere with the CLL drug. You might think such errors would be prevented by expert medical oversight or the software for ordering medications. Make no assumptions; question everything.
Final Thoughts
Having the attitude of an active self-manager of one’s medical treatment is necessary but not sufficient. You have to be effective. The attitude motivates vigilance, inquisitiveness, and assertiveness. But to guide and channel those resources, you need relevant, detailed knowledge.
In addition to knowing the way things are, you need to know how to get things done: How to identify drug interactions, or to politely but firmly tell the nurse or phlebotomist that your IV has expired, that you’d rather their glove not be “modified,” or that you no longer want them to work with you. Being a well-informed, active self-manager of your medical treatment could save your life.
Dr. Richard Contrada is a health psychologist at Rutgers where he directs the Social, Health, and Interdisciplinary Psychophysiology Lab and whose research has addressed the role of stress in cardiovascular disease among other topics. He has published over 100 articles, papers, and edited volumes, the latter including The Handbook of Stress Science: Biology, Psychology, and Health.




